
Skeletal Tissue (Bone and Cartilage)
INTRODUCTORY COMMENTS
Several varieties of specialized connective tissue together form the skeleton.
Appreciating the composition of these tissues is important for understanding
the mechanical properties of the skeleton and its susceptibility to various
types injury. Furthermore, understanding the processes of normal (and
abnormal) skeletal development, of healing after injury, and of degeneration
requires some knowledge of the cells which produce these tissues.
Bone and cartilage, like all other connective tissues,
consist of cells and extracellular matrix. It is the ground
substance of the matrix which is
most responsible for the conspicuous differences between bone and cartilage.
The ground substance of bone
is mineralized, making the bone rigid and strong, but brittle. The ground
substance of cartilage is not mineralized but is more like very
firm Jello®, making cartilage stiff and incompressible but more
flexible and resilient than bone.
Yet, in spite of their solidity, both bone and cartilage are capable of growth.
In the case of bone, internal remodelling
(essentially, ongoing destruction and renewal) is an active process throughout
life.
In both cartilage and bone, the microscopic appearance of ground substance
tends to obscure the presence of collagen. However, as in most other connective tissues
(other than blood), collagen is a principal
fibrous component which confers tensile strength. (The exceptionally
flexible cartilage of ears and epiglottis is also heavily invested with elastin.)
CLINICAL NOTE: A balance between osteoclast
and osteoblast activity is necessary for a stable calcium
level in blood. To this end, osteoclast activity is hormonally regulated,
stimulated by parathyroid hormone and inhibited by calcitonin
from C-cells of the thyroid.
TOP OF PAGE
Clinical relevance of skeletal tissue histology
Broken bones heal by an acceleration of the normally ongoing process of bone remodeling.
The break is first patched by formation of new primary (woven) bone and is then gradually reshaped
to approximate the bone's original texture and strength.
Initial treatment for broken bones usually involves basic mechanical considerations,
stabilizing the structure to prevent further injury. And of course some
breaks, such as cervical fracture, immediately raise urgent neurological concerns.
But optimizing subsequent repair (which should minimize long-term impairment)
requires some considerable understanding of the mechanical properties and
healing process of bone and cartilage.
Because we do not have slides of broken and healing bone, the various aspects
of bone structure, growth and remodelling must be observed piecemeal in other
specimens.
Bone which has been remodelled, or which was originally laid down on a neat
preexisting bony surface, displays a pattern called lamellar bone.
Bone that has been created without such a surface, as in initial repair
of a fracture, is less well organized and is described as primary or
woven bone.
TOP OF PAGE
SLIDE GUIDE: What can be seen, and what should be noticed, on selected
slides from the reference set. Each of these slides shows some feature
of skeletal tissues. (LUMEN has
"Zoomify" slides that are similar to several of these.)
Note: All slides of bone in our slide-set, EXCEPT those labelled "Ground Bone,"
represent decalcified bone from which the mineral has been removed, while
leaving behind cells and organic matrix.]
Ground Bone, x.s.
Gound Bone, l.s.
Decalcified Bone (rabbit femur), x.s. or l.s.
Developing Cartilage Bone
Trachea and lung
Fibrocartilage
Elastic Cartilage
Hyaline Cartilage
Early Dental Cup
Internal Ear
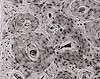
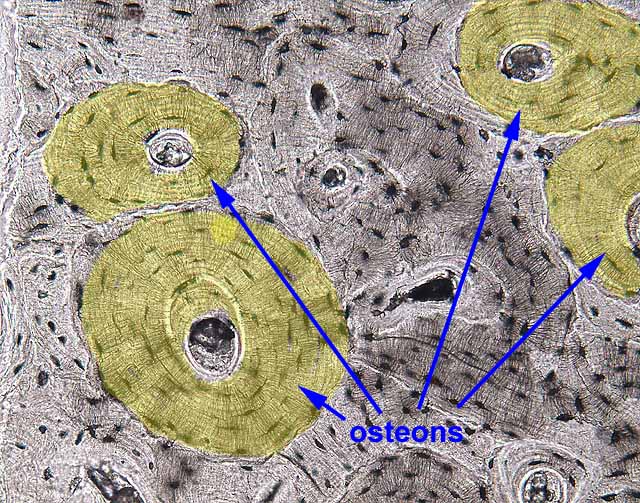
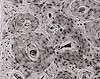 Our "ground bone" slide displays a piece of bone from which all
organic material has been removed and the remaining mineral matrix prepared
by grinding a small chip of bone into a slab thin enough to transmit light
(hence "ground bone," where "ground" is the past-tense
of "grind"). The gritty texture which may be observed within
most Haversian canals of these specimens is bone dust, an
artifact of this preparation by grinding.
Our "ground bone" slide displays a piece of bone from which all
organic material has been removed and the remaining mineral matrix prepared
by grinding a small chip of bone into a slab thin enough to transmit light
(hence "ground bone," where "ground" is the past-tense
of "grind"). The gritty texture which may be observed within
most Haversian canals of these specimens is bone dust, an
artifact of this preparation by grinding.
The two slides ("x.s." vs. "l.s.") differ only in plane
of section -- the cross section ("x.s.") displays concentric lamellae
surrounding Haversian canals; the longitudinal section ("l.s.")
shows how the lamellae and canals run longitudinally along the long axis
of the bone. Both slides display lacunae with interconnecting canaliculi.
Since canaliculi are NOT normally visible in decalcified bone, these
are our best slides for observing these channels. [Exercise: On
a cross section of "ground bone," try to reason out which lamellar
systems were formed most recently and which pieces represent the oldest
relics of former osteons; see remodelling below.]
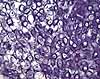
 The
slide labelled "rabbit femur" displays decalcified bone from
which the mineral has been removed, leaving behind cells and organic matrix.
The section may be either cross section ("x.s.") or longitudinal
section ("l.s."). Most features of bone (but not the canaliculi,
which are only visible on ground bone) may be found on these
slides, which include not only bone but also bone marrow (on the inside) and
often periosteum and muscle (on the outside). Active remodelling
is apparent on some of these slides (evident by the presence of active osteoblasts
and osteoclasts), but the others display quiescent bone. Some
of the slides showing active remodelling also display some blue-stained patches
within the otherwise-eosinophilic bone; these represent remnants of calcified
cartilage which has not yet been replaced by bone.
The
slide labelled "rabbit femur" displays decalcified bone from
which the mineral has been removed, leaving behind cells and organic matrix.
The section may be either cross section ("x.s.") or longitudinal
section ("l.s."). Most features of bone (but not the canaliculi,
which are only visible on ground bone) may be found on these
slides, which include not only bone but also bone marrow (on the inside) and
often periosteum and muscle (on the outside). Active remodelling
is apparent on some of these slides (evident by the presence of active osteoblasts
and osteoclasts), but the others display quiescent bone. Some
of the slides showing active remodelling also display some blue-stained patches
within the otherwise-eosinophilic bone; these represent remnants of calcified
cartilage which has not yet been replaced by bone.
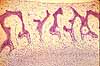
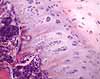
 The
slide labelled "developing cartilage bone" displays a longitudinal
section through the end of a long bone, at a fairly youthful stage in development
when only the shaft (diaphysis) has been mineralized and the end is still
cartilagenous. The slide illustrates the process of endochondral
ossification (in which cartilage is growing outward toward the end of
the bone, while bone tissue is following along behind, invading and replacing
the cartilage. In addition to endochondral ossification, you can of
course also see hyaline cartilage (the cartilage which faces the articular
surface), trabecular bone, cortical bone, bone marrow, muscle, and usually
some active osteoblasts and osteoclasts (already remodelling the freshly formed
bone). Some of the slides include ends of two bones meeting at a synovial
joint, with endochondral ossification occurring in the ends of both long
bones.
The
slide labelled "developing cartilage bone" displays a longitudinal
section through the end of a long bone, at a fairly youthful stage in development
when only the shaft (diaphysis) has been mineralized and the end is still
cartilagenous. The slide illustrates the process of endochondral
ossification (in which cartilage is growing outward toward the end of
the bone, while bone tissue is following along behind, invading and replacing
the cartilage. In addition to endochondral ossification, you can of
course also see hyaline cartilage (the cartilage which faces the articular
surface), trabecular bone, cortical bone, bone marrow, muscle, and usually
some active osteoblasts and osteoclasts (already remodelling the freshly formed
bone). Some of the slides include ends of two bones meeting at a synovial
joint, with endochondral ossification occurring in the ends of both long
bones.
 The
slide labelled "fibrocartilage" displays considerably more
than fibrocartilage. It appears to be a section through the pubic symphysis,
with a more-or-less symmetrical arrangement of bone and muscle on either side
of the midline, with the bones bound together by a fibrocartilagenous joint
in the medial region of the preparation. Although collagen is present
in all cartilage, microscopically visible strands are only apparent in fibrocartilage,
where they contribute extra toughness. Active remodelling may be apparent in
the bone on this slide (as evidenced by the presence of active osteoblasts
and osteoclasts).
The
slide labelled "fibrocartilage" displays considerably more
than fibrocartilage. It appears to be a section through the pubic symphysis,
with a more-or-less symmetrical arrangement of bone and muscle on either side
of the midline, with the bones bound together by a fibrocartilagenous joint
in the medial region of the preparation. Although collagen is present
in all cartilage, microscopically visible strands are only apparent in fibrocartilage,
where they contribute extra toughness. Active remodelling may be apparent in
the bone on this slide (as evidenced by the presence of active osteoblasts
and osteoclasts).

 Slides of "trachea" and "trachea and esophagus"
display the C-shaped
rings of cartilage that reinforce the trachea. Cartilage may also be
found in bronchial walls in the slide of "lung".
Slides of "trachea" and "trachea and esophagus"
display the C-shaped
rings of cartilage that reinforce the trachea. Cartilage may also be
found in bronchial walls in the slide of "lung".
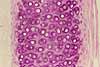
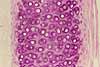
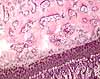
 The
slides of "hyaline cartilage" and "elastic cartilage"
simply display examples of these two tissue types without much context. The
source for the hyaline cartilage is not obvious; the elastic cartilage example
may be from epiglottis (deducing from the appearance of the associated epithelium).
The elastic cartilage slide is stained for elastin (the fine purple
strands within the matrix); otherwise it would look just like hyaline cartilage.
Hyaline cartilage may be seen on several other slides, notably
"developing cartilage bone," "early dental cup," and "trachea."
The
slides of "hyaline cartilage" and "elastic cartilage"
simply display examples of these two tissue types without much context. The
source for the hyaline cartilage is not obvious; the elastic cartilage example
may be from epiglottis (deducing from the appearance of the associated epithelium).
The elastic cartilage slide is stained for elastin (the fine purple
strands within the matrix); otherwise it would look just like hyaline cartilage.
Hyaline cartilage may be seen on several other slides, notably
"developing cartilage bone," "early dental cup," and "trachea."
 The
slide labelled "early dental cup" displays many features
of facial development in a section across the snout of an unidentified animal
fetus. If you enjoy microscopy, figuring out this slide should be fun.
Symmetry about the midline should help you get oriented. You
can then find major anatomical features such as the tongue (with its texture
of crisscrossing muscle fibers), the nasal septum (hyaline cartilage), the
jaw, and various skull bones. You can then examine the appearance of
various bones in various stages of intramembranous or endochondral ossification.
You may also find developing muscles, teeth, salivary glands, and skin.
The
slide labelled "early dental cup" displays many features
of facial development in a section across the snout of an unidentified animal
fetus. If you enjoy microscopy, figuring out this slide should be fun.
Symmetry about the midline should help you get oriented. You
can then find major anatomical features such as the tongue (with its texture
of crisscrossing muscle fibers), the nasal septum (hyaline cartilage), the
jaw, and various skull bones. You can then examine the appearance of
various bones in various stages of intramembranous or endochondral ossification.
You may also find developing muscles, teeth, salivary glands, and skin.
 The
slide of "internal ear" displays the many elaborate structures
of the inner ear, all embedded in bone. This is also the only slide
we have in which some of bone has no obvious lamellar pattern, suggesting
it represents primary or woven bone that has not yet been replaced
by remodelling. If finding and seeing that sounds exciting to you, then
enjoy; but you should first become acquainted with the appearance of bone
in other specimens (listed above) which are not as complex.
The
slide of "internal ear" displays the many elaborate structures
of the inner ear, all embedded in bone. This is also the only slide
we have in which some of bone has no obvious lamellar pattern, suggesting
it represents primary or woven bone that has not yet been replaced
by remodelling. If finding and seeing that sounds exciting to you, then
enjoy; but you should first become acquainted with the appearance of bone
in other specimens (listed above) which are not as complex.
TOP OF PAGE
CARTILAGE
The ground substance of cartilage
is characterized by a firm solid gel-like matrix (rather like very firm Jello®)
reinforced by collagen. Cartilage
is relatively stiff and incompressible. However, since cartilage is
not mineralized, it is more flexible and resilient than bone.
 The
characteristic microscopic texture of cartilage, with cells enclosed
in individual lacunae (small chambers), reflects the nature of cartilage
matrix and its mode of formation. While cartilage is growing, new
cartilage matrix is secreted by chondroblasts, which become isolated
from one another as the matrix is formed. As more matrix is secreted,
these chondroblasts are pushed farther apart. Chondroblasts divide
within their lacunae to form "isogenous cell clusters," which then
form more matrix and become separated from one another. Once growth
ceases, the resting cells are called chondrocytes. Although apparently
quiescent, chondrocytes continue to interact at a molecular level with cartilage
matrix (e.g., by recycling aggrecan, a major proteoglycan in the matrix.).
The
characteristic microscopic texture of cartilage, with cells enclosed
in individual lacunae (small chambers), reflects the nature of cartilage
matrix and its mode of formation. While cartilage is growing, new
cartilage matrix is secreted by chondroblasts, which become isolated
from one another as the matrix is formed. As more matrix is secreted,
these chondroblasts are pushed farther apart. Chondroblasts divide
within their lacunae to form "isogenous cell clusters," which then
form more matrix and become separated from one another. Once growth
ceases, the resting cells are called chondrocytes. Although apparently
quiescent, chondrocytes continue to interact at a molecular level with cartilage
matrix (e.g., by recycling aggrecan, a major proteoglycan in the matrix.).
Disturbance of matrix maintenance by chondrocytes is implicated
osteoarthritis and in Kashin-Beck disease (KBD; see
Science 324:1378, 2009).
Since cartilage is avascular, as the cartilage increases in bulk,
its cells also grow farther and farther from their source of nutrition. As
a direct result, mature cartilage is a relatively inactive tissue with minimal
ability to respond to injury. Nevertheless, cartilage remains a living
tissue (as does bone): Healthy chondrocytes are necessary to maintain the
molecular integrity of the cartilage matrix.
Three forms of cartilage are conventionally recognized:
- Hyaline cartilage, the most common form, is a precursor to developing bone
and is also found in synovial joints and as reinforcement for trachea and bronchi.
- Fibrocartilage, reinforced for toughness with collagen fibers, is found in intervertebral discs as well as the pubic symphysis.
- Elastic cartilage, more flexible and springy, is found in ear and epiglottis.
- A fourth type, lipocartilage, has recently been recognized.
 Hyaline
cartilage may be observed in several slides from your reference set, not
just the one labelled "hyaline cartilage." Also examine the trachea
and the cartilage precursors of bone in the slides of developing bone and
skull. The latter slide, which may be labelled "early dental cup," is
a section across the snout of a fetal rat or pig.
Hyaline
cartilage may be observed in several slides from your reference set, not
just the one labelled "hyaline cartilage." Also examine the trachea
and the cartilage precursors of bone in the slides of developing bone and
skull. The latter slide, which may be labelled "early dental cup," is
a section across the snout of a fetal rat or pig.
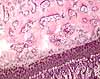
 Fibrocartilage
is exemplified in your slide set by a section of the pubic symphysis. Fibrocartilage
may be seen in the medial region of this symmetrical preparation, characterized
by visible bands of eosinophilic collagen.
(In hyaline cartilage, in contrast, the fine collagen filaments
throughout the matrix do not stain with routine H&E.)
The cells in their lacunae tend to line up in rows between the eosinophilic
bands of collagen, but are otherwise similar to those in hyaline cartilage.
Fibrocartilage
is exemplified in your slide set by a section of the pubic symphysis. Fibrocartilage
may be seen in the medial region of this symmetrical preparation, characterized
by visible bands of eosinophilic collagen.
(In hyaline cartilage, in contrast, the fine collagen filaments
throughout the matrix do not stain with routine H&E.)
The cells in their lacunae tend to line up in rows between the eosinophilic
bands of collagen, but are otherwise similar to those in hyaline cartilage.
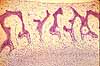
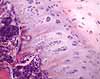
 With
routine H&E stain, elastic cartilage looks like hyaline cartilage, with
the same appearance of clustered cells in lacunae. Grossly, the tissue
is yellowish because of the presence of elastin.
The elastin can also be demonstrated by special staining, as in the
reference set slide of "elastic cartilage."
With
routine H&E stain, elastic cartilage looks like hyaline cartilage, with
the same appearance of clustered cells in lacunae. Grossly, the tissue
is yellowish because of the presence of elastin.
The elastin can also be demonstrated by special staining, as in the
reference set slide of "elastic cartilage."
Lipocartilage, found in the ears, nose and throat, is based on fat-filled cells called
"lipochondrocytes"
that allow the tissue to remain soft and springy, "similar to bubbled packaging material." Lipocartilage has only been recently (re)discovered by Raul Ramos et al., after having been first described by Franz von Leydig in 1854. (For a nice summary, see Science 387:136-137, 9 Jan. 2025)
TOP OF PAGE
BONE
Perhaps the most surprising attribute of bones, at least for beginners, is that bones are alive.
Bones are not just dead, mineralized structural elements. The material of bone is constantly being worked-over
(remodelled) through the activities of the cells contained within. And this
ongoing activity is an essential part of the body's overall metabolism, maintaining appropriate calcium ion concentrations
throughout the body.
The composition and histological organization of bone are well-described
in most histology books. (REMINDER: Using this
website should not be a substitute for reading a real textbook.) What follows is primarily a guide to observing
particular features microscopically.
Most of the significant features of bone can be observed in your reference
slides, but not every feature will be apparent on every slide. To properly
appreciate each slide, you need to realize whether the bone is still developing
(i.e., with sites of endochondral or intramembranous ossification) or mature,
and also to determine whether or not active remodelling is visible.
Most mature bones are more-or-less hollow. (Within the hollow is bone marrow.)
The outer bone is called cortical or compact bone, while the inner marrow cavity may
be criss-crossed by thin strands of bone called trabeculae.

Well-formed Haversian systems are best displayed on our slides of
"ground bone." They will not be found in primary,
or woven, bone (bone which has not yet undergone remodelling),
examples of which may be observed in some of our slides of "internal
ear" (in the bony labyrinth around the cochlea).
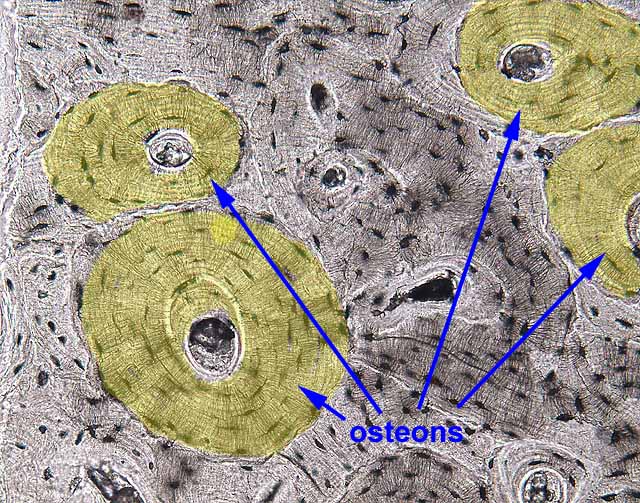
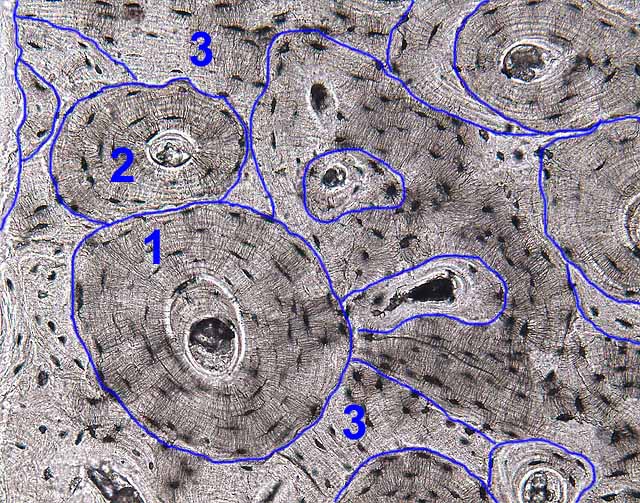
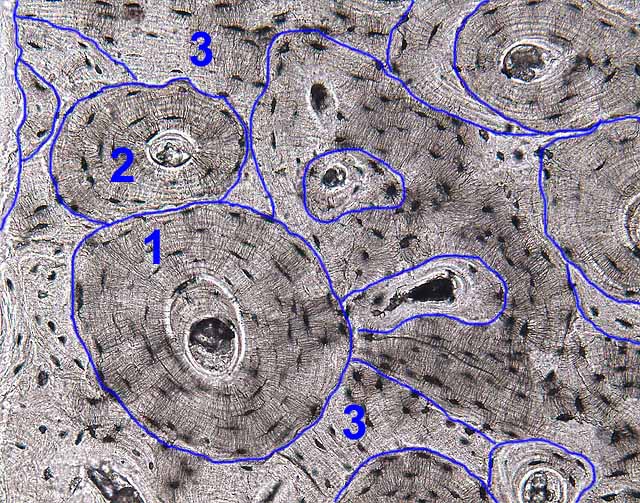
In any bone with well-developed lamellae, only some of the lamellae will appear
as neat concentric Haversian systems (i.e., with a roughly circular outline
and a Haversian canal in the center). Other lamellae appear to form
only partial osteons, with some portion replaced by the more well-formed
lamellae of an adjacent osteon. Still more lamellae appear only as
haphazard pieces, with no central canal. This pattern of overlapping
osteons and fragmentary lamellar systems provides a visible record of past
and recent remodelling.
 Exercise:
On a cross section of "ground bone," try to reason
out which lamellar systems were formed most recently and which pieces represent
the oldest relics of former osteons.
Exercise:
On a cross section of "ground bone," try to reason
out which lamellar systems were formed most recently and which pieces represent
the oldest relics of former osteons.

 Other slides of bone in your reference set ("rabbit femur," "fibrocartilage,"
"inner ear") represent decalcified tissue, in which details of cells
are visible. Collagen in the matrix is left intact by
the decalcification process, so the bone matrix appears eosinophilic (i.e.,
pink in H&E-stained material).
Matrix details (especially canaliculi) are less apparent than
in ground bone. In mature resting bone, including the slide of
"rabbit femur," osteoclasts are rare and osteoblasts are represented
only by small, inactive bone-lining cells. Both of these cell types
can be readily found in their active states in the slide of "developing cartilage
bone," where bone is being actively resorbed and laid down, and also in the
slide of "fibrocartilage."
Other slides of bone in your reference set ("rabbit femur," "fibrocartilage,"
"inner ear") represent decalcified tissue, in which details of cells
are visible. Collagen in the matrix is left intact by
the decalcification process, so the bone matrix appears eosinophilic (i.e.,
pink in H&E-stained material).
Matrix details (especially canaliculi) are less apparent than
in ground bone. In mature resting bone, including the slide of
"rabbit femur," osteoclasts are rare and osteoblasts are represented
only by small, inactive bone-lining cells. Both of these cell types
can be readily found in their active states in the slide of "developing cartilage
bone," where bone is being actively resorbed and laid down, and also in the
slide of "fibrocartilage."
BONE CELLS
 Three functionally distinct cell types can be recognized in bone: osteocytes, osteoblasts,
and osteoclasts.
Three functionally distinct cell types can be recognized in bone: osteocytes, osteoblasts,
and osteoclasts.
- Osteocytes are small, inactive cells, seemingly isolated
from one another in individual lacunae. Inconspicuous cell processes
extend out through tiny canaliculi and provide gap-junctional contact among
neighboring osteocytes as a means of communication and nutrient supply through
the otherwise-impermeable bone matrix.
- Osteoblasts (bone-forming cells) are small cuboidal cells,
usually found lying adjacent to one another upon lamellae they have just
secreted. (A row of osteoblasts can superficially resemble a simple cuboidal epithelium.)
- Osteoblasts lay down new bone lamellae. They are active during bone
development and also during bone remodelling.
- Inactive osteoblasts may be called "bone-lining cells."
 Populations
of osteocytes and osteoblasts may be interchangeable, reflecting different
stages in the activity of individual cells. That is, active osteoblasts
that become enclosed in bone may adopt the resting osteocyte form, while
osteocytes which are released from their bony matrix (by osteoclast
activity) may become active osteoblasts.
Populations
of osteocytes and osteoblasts may be interchangeable, reflecting different
stages in the activity of individual cells. That is, active osteoblasts
that become enclosed in bone may adopt the resting osteocyte form, while
osteocytes which are released from their bony matrix (by osteoclast
activity) may become active osteoblasts.
- Osteoclasts (bone-removing cells) are large cells with multiple
nuclei, each one typically sitting alone within a small hollow called a "Howship's
lacuna" (the name commemorates John
Howship, b. 1781). These lacunae are created by the osteoclasts
themselves, as they remove adjacent
bone matrix during remodelling.
- Osteoclasts remove preexisting bone. They are active in bone
development and also in bone remodelling.
- Osteoclasts are more closely related to macrophages than to osteocytes
or osteoblasts. They form a distinct cell population derived from
the same precursor cells as macrophages.
These three cell types can be identified not only by their appearance as cells but also by their
position in relation to the adjacent bone lamellae:
- Osteocytes are isolated within lacunae, separated from other cells
by intervening bone matrix.
- Osteoblasts occur along a surface which parallels the lamellae
that they are producing.
- Osteoclasts occur in small hollows (called Howship's lacunae)
which they have eroded into the surface. The edges of these hollows
typically cut across the underlying lamellae.
CLINICAL NOTE: A balance between osteoclast
and osteoblast activity is necessary for a stable calcium
level in blood. To this end, osteoclast activity is hormonally regulated,
stimulated by parathyroid hormone and inhibited by calcitonin
from C-cells of the thyroid.
TOP OF PAGE
BONE MARROW
Don't neglect to notice the specialized connective tissues which fill the
marrow cavity of many bones, including both
hemopoietic (blood-forming) tissue and fat.
Bone marrow is not described in this website.
TOP OF PAGE
DEVELOPMENT and REMODELLING of Skeletal Tissues
Cartilage formation
 Cartilage
forms from initial condensation directly from mesenchyme and then grows by
a combination of apositional growth (additional of new cells and matrix
onto the outside of the growing structure) and interstitial expansion
(cell division and secretion of new matrix within an established structure).
The cells which form cartilage are called chondroblasts; resting (i.e.,
non-growing) cartilage cells are called chondrocytes. Because
chondroblasts cannot move freely through the cartilage matrix, they tend to
form clusters, called isogenous groups, at the sites where they divide.
Cartilage
forms from initial condensation directly from mesenchyme and then grows by
a combination of apositional growth (additional of new cells and matrix
onto the outside of the growing structure) and interstitial expansion
(cell division and secretion of new matrix within an established structure).
The cells which form cartilage are called chondroblasts; resting (i.e.,
non-growing) cartilage cells are called chondrocytes. Because
chondroblasts cannot move freely through the cartilage matrix, they tend to
form clusters, called isogenous groups, at the sites where they divide.
|
Growth of cartilage, from Blue
Histology (Copyright
Lutz Slomianka 1998-2004)
(The image should be animated, if
you watch patiently.)
 Growth
occurs by two mechanisms. Growth
occurs by two mechanisms.
- Interstitial growth - Chondroblasts within the existing
cartilage divide and form small groups of cells, isogenous groups,
which produce matrix to become separated from each other by a thin
partition of matrix. Interstitial growth occurs mainly in immature
cartilage.
- Appositional growth - Mesenchymal cells surrounding the cartilage
in the deep part of the perichondrium (or the chondrogenic layer)
differentiate into chondroblasts. Appositional growth occurs also
in mature cartilage.
In the animation, chondroblast cytoplasm
is red, chondroblast
nuclei are blue, and cartilage
matrix is gray.
|
Mature cartilage is avascular and relatively permanent. (This is in contrast to
mature bone, which is highly vascular and whose extracellular material is continually
being remodeled by the cells within, even in adults.) The functional
properties of cartilage are derived from relatively stable extracellular materials,
not from any ongoing cellular activity. Once cartilage has formed, it
is pretty much finished (although it may continue to expand with age and become
somewhat less resilient). If adult cartilage is damaged, it may be replaced
not by new cartilage but by collagenous scarring. This is especially
significant in case of damage to articular cartilages in joints.
 Bone
formation
Bone
formation
Bone develops embryonically in two different
ways -- either by intramembranous ossification (directly from mesenchymal
condensations) or by endochondral ossification (by transformation of
a pre-existing cartilagenous model). Once bones are initially developed,
bone continually undergoes a process of remodelling
in which old bone is removed and replaced by newly-formed bone.
INTRAMEMBRANOUS OSSIFICATION
 The
simpler mode of bone formation is intramembranous, in which bone forms directly
in mesenchyme. This is the pattern for the thin, flat bones of
the skull (hence, "intramembranous"). During intramembranous
bone formation, ossification occurs in spicules around mesenchymal vessels.
Spicules of bone covered by osteoblasts, may be observed in the "dental
cup" slide, which shows the snout of a young animal.
The
simpler mode of bone formation is intramembranous, in which bone forms directly
in mesenchyme. This is the pattern for the thin, flat bones of
the skull (hence, "intramembranous"). During intramembranous
bone formation, ossification occurs in spicules around mesenchymal vessels.
Spicules of bone covered by osteoblasts, may be observed in the "dental
cup" slide, which shows the snout of a young animal.
 ENDOCHONDRAL
OSSIFICATION
ENDOCHONDRAL
OSSIFICATION
Most of the embryonic skeleton forms initially as cartilage.
During endochondral ossification, osteoblasts and blood vessels must actually
invade the cartilage precursor. In long bones (e.g., tibia, humerus),
a plate of cartilage remains through adolescence at the junction between epiphysis
and diaphysis. This epiphyseal plate is the site of bone elongation,
with new cartilage forming on the epiphyseal side of the plate while endochondral
ossification extends the diaphysis on the other side of the plate. This
arrangement allows the epiphyseal ends of the bone to be solidly calcified
(and hence able to bear the brunt of the forces the bone experiences) even
while the bone is still growing. Eventually, the ossification front
catches up with the chondrogenic front, all of the cartilage is replace by
bone, and bone elongation ceases. Timing of this occurrence varies with
some predictability from bone to bone and thus contributes to the forensic
determination of the age of death from from skeletal remains.
 On
your reference slide labelled "developing cartilage bone,"
you can observe endochondral bone formation in the epiphyseal region of a
long bone. The entire process, from proliferating chondroblasts,
through expanding and hypertrophic cartilage, to mineralization of the cartilage,
invasion by blood vessels and osteoblasts,
On
your reference slide labelled "developing cartilage bone,"
you can observe endochondral bone formation in the epiphyseal region of a
long bone. The entire process, from proliferating chondroblasts,
through expanding and hypertrophic cartilage, to mineralization of the cartilage,
invasion by blood vessels and osteoblasts,
 and remodelling by osteoclasts, can seen sequentially by
scanning from the epiphysis toward the diaphysis. A continually advancing
growth front has established the appearance of a "layered" structure that
is really just a series of points caught at different stages within the same
process.
and remodelling by osteoclasts, can seen sequentially by
scanning from the epiphysis toward the diaphysis. A continually advancing
growth front has established the appearance of a "layered" structure that
is really just a series of points caught at different stages within the same
process.
The process of endochondral ossification may also be observed at a synarthrosis
in the slide labelled "fibrocartilage."
Bone Remodelling
Living bone is continually being remodelled -- essentially, the matrix is
constantly being removed and rebuilt. The process of bone remodelling
is extremely active during childhood (maintaining the shape of each bone as
the body grows larger) but slows down with advancing age.
 During
body growth, bones can change shape as well as size. To accomplish this,
bone matrix is removed on one surface (by osteoclasts)
while bone matrix is being added on another surface (by osteoblasts).
During
body growth, bones can change shape as well as size. To accomplish this,
bone matrix is removed on one surface (by osteoclasts)
while bone matrix is being added on another surface (by osteoblasts).
|
Reorganisation and Restoration of Bone, from Blue
Histology (Text and GIF copyright
Lutz Slomianka 1998-2004)
(The image should be animated, if
you watch patiently.)
 Changes
in the size and shape of bones during the period of growth imply some
bone reorganisation. Osteoblasts and osteoclasts constantly deposit
and remove bone to adjust its properties to growth-related demands on
size and/or changes of tensile and compressive forces. Changes
in the size and shape of bones during the period of growth imply some
bone reorganisation. Osteoblasts and osteoclasts constantly deposit
and remove bone to adjust its properties to growth-related demands on
size and/or changes of tensile and compressive forces.
In the animation, osteoclasts are
pink, osteoblasts
are blue, and lamellae
are gray.
Osteocytes (within the lamellae) are not shown.
Although the reorganisation of bone may not result in macroscopically
visible changes of bone structure, it continues throughout life to mend
damage to bone (e.g. microfractures) and to counteract the wear and
tear occurring in bone. Osteoclasts and osteoblasts remain the
key players in this process. Osteoclasts "drill" more or less
circular tunnels within existing bone matrix. Osteoblasts deposit
new lamellae of bone matrix on the walls of these tunnels resulting
in the formation of a new Haversian system within the matrix of compact
bone. Parts of older Haversian systems, which may remain between
the new ones, represent the interstitial lamellae in mature bone.
Capillaries and nerves sprout into new Haversian canals.
Restorative activity continues in aged humans (about 2% of the Haversian
systems seen in an 84 year old individual contained lamellae that had
been formed within 2 weeks prior to death!). However, the Haversian
systems tend to be smaller in older individuals and the canals are larger
because of slower bone deposition. If these age-related changes
in the appearance of the Haversian systems are pronounced they are termed
osteopenia or senile osteoporosis. The reduced strength of bone
affected by osteoporosis will increase the likelihood of fractures.
|
The lamellar texture of bone is a direct result of remodeling. Broken
bones heal by an acceleration of the normally ongoing process of bone remodeling.
The break is first patched by formation of new primary (woven) bone
and is then gradually reshaped to approximate the bone's original texture and strength.
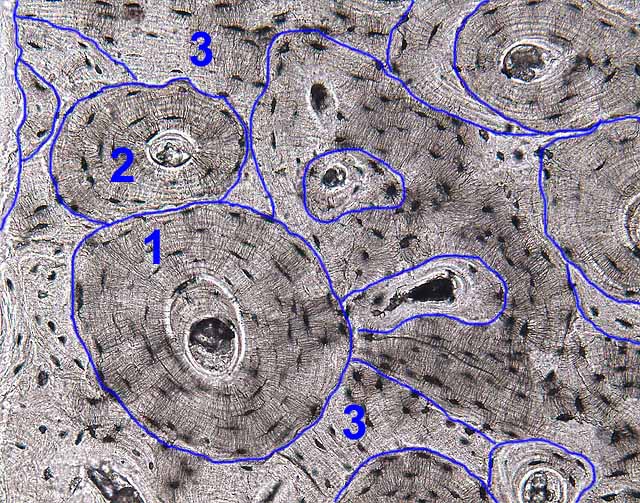 The
entire lamellar structure of mature bone is best understood as the result
of bone remodeling. During remodelling, osteoclasts
travel along a vessel resorbing some of the existing bone to form a relatively
large tunnel. Following along behind are osteoblasts
which then lay down a neat new set of Haversian lamellae encircling the vessel,
upon a cement line that marks the limit of resorption. The process repeats
indefinitely, with fragments of the lamellae from older Haversian systems
being left behind as interstitial lamellae when new systems are formed.
The
entire lamellar structure of mature bone is best understood as the result
of bone remodeling. During remodelling, osteoclasts
travel along a vessel resorbing some of the existing bone to form a relatively
large tunnel. Following along behind are osteoblasts
which then lay down a neat new set of Haversian lamellae encircling the vessel,
upon a cement line that marks the limit of resorption. The process repeats
indefinitely, with fragments of the lamellae from older Haversian systems
being left behind as interstitial lamellae when new systems are formed.
CLINICAL NOTE: A balance between osteoclast
and osteoblast activity is necessary for a stable calcium
level in blood. To this end, osteoclast activity is hormonally regulated,
stimulated by parathyroid hormone and inhibited by calcitonin
from C-cells of the thyroid.
 Remodelling
can be observed in the reference slides labelled "developing
cartilage bone" and "fibrocartilage"
(not in the cartilage, of course, but in the adjacent bone), and also in some
but not all of the slides labelled "rabbit femur."
The "fossils" of remodelling (patterns of Haversian lamellae that
have been partially obliterated by subsequent osteoclast activity) may be
observed in any bone slide, perhaps most clearly in "ground
bone."
Remodelling
can be observed in the reference slides labelled "developing
cartilage bone" and "fibrocartilage"
(not in the cartilage, of course, but in the adjacent bone), and also in some
but not all of the slides labelled "rabbit femur."
The "fossils" of remodelling (patterns of Haversian lamellae that
have been partially obliterated by subsequent osteoclast activity) may be
observed in any bone slide, perhaps most clearly in "ground
bone."
TOP OF PAGE
JOINTS
Joints and associated tissues develop from mesenchyme and may be classified
as specialized connective tissue, like other skeletal structures. They
are variously composed of fibrocollagenous tissue (principally collagen and
fibroblasts) or cartilage. You should appreciate the mechanical differences
associated with different types of joint tissue, and be familiar with some
specific examples of each type.
 The
synarthrosis joint type is represented in our reference slide set by
the fibrocartilage of the pubic symphysis.
The
synarthrosis joint type is represented in our reference slide set by
the fibrocartilage of the pubic symphysis.
Synovial joints have the most specialized structure. The synovial
lining is formed from hyaline collagen and synovial cells with no basement
membrane. The synovial cavity is thus not lined by a proper epithelium
but is more like a highly specialized intercellular space in connective
tissue. The synovial fluid is an interstitial fluid, an ultrafiltrate
from synovial capillaries, together with highly polymerized hyaluronic acid
and glycoprotein secreted by the fibroblast-like synovial cells. This
fluid exudes from the synovial membrane and is apparently responsible both
for lubricating and nourishing the articular cartilages.
There are normally few white blood cells in the synovial
fluid (less than 300 / mm3 vs. about 5000 / mm3 for blood). A significant
increase in this number is indicative of joint disease.
The synovium is susceptible to various forms of damage,
for example in rheumatoid arthritis.
In our slide sets, some of the slides of developing
cartilage bone include the end of an adjacent bone and, between the two, a
synovial joint. You can examine various other joints grossly
in anatomy lab.
TOP OF PAGE
SKELETAL PATHOLOGY
Bone repair (after a break that has been neatly re-set) takes place by a process similar to that of bone remodelling, hopefully resulting freshly-formed bone that eventually is at least as strong as the original. Details of skeletal pathology should be available in any pathology
text (e.g., Robbin's Pathological Basis of Disease).
TOP OF PAGE
Comments and questions: dgking@siu.edu
SIUC / School
of Medicine / Anatomy / David
King
https://histology.siu.edu/ssb/skeleton.htm
Last updated: 9 February 2025 / dgk
 Our "ground bone" slide displays a piece of bone from which all
organic material has been removed and the remaining mineral matrix prepared
by grinding a small chip of bone into a slab thin enough to transmit light
(hence "ground bone," where "ground" is the past-tense
of "grind"). The gritty texture which may be observed within
most Haversian canals of these specimens is bone dust, an
artifact of this preparation by grinding.
Our "ground bone" slide displays a piece of bone from which all
organic material has been removed and the remaining mineral matrix prepared
by grinding a small chip of bone into a slab thin enough to transmit light
(hence "ground bone," where "ground" is the past-tense
of "grind"). The gritty texture which may be observed within
most Haversian canals of these specimens is bone dust, an
artifact of this preparation by grinding.  The
slide labelled "rabbit femur" displays decalcified bone from
which the mineral has been removed, leaving behind cells and organic matrix.
The section may be either cross section ("x.s.") or longitudinal
section ("l.s."). Most features of bone (but not the canaliculi,
which are only visible on ground bone) may be found on these
slides, which include not only bone but also bone marrow (on the inside) and
often periosteum and muscle (on the outside). Active remodelling
is apparent on some of these slides (evident by the presence of active osteoblasts
and osteoclasts), but the others display quiescent bone. Some
of the slides showing active remodelling also display some blue-stained patches
within the otherwise-eosinophilic bone; these represent remnants of calcified
cartilage which has not yet been replaced by bone.
The
slide labelled "rabbit femur" displays decalcified bone from
which the mineral has been removed, leaving behind cells and organic matrix.
The section may be either cross section ("x.s.") or longitudinal
section ("l.s."). Most features of bone (but not the canaliculi,
which are only visible on ground bone) may be found on these
slides, which include not only bone but also bone marrow (on the inside) and
often periosteum and muscle (on the outside). Active remodelling
is apparent on some of these slides (evident by the presence of active osteoblasts
and osteoclasts), but the others display quiescent bone. Some
of the slides showing active remodelling also display some blue-stained patches
within the otherwise-eosinophilic bone; these represent remnants of calcified
cartilage which has not yet been replaced by bone.  The
slide labelled "developing cartilage bone" displays a longitudinal
section through the end of a long bone, at a fairly youthful stage in development
when only the shaft (diaphysis) has been mineralized and the end is still
cartilagenous. The slide illustrates the process of endochondral
ossification (in which cartilage is growing outward toward the end of
the bone, while bone tissue is following along behind, invading and replacing
the cartilage. In addition to endochondral ossification, you can of
course also see hyaline cartilage (the cartilage which faces the articular
surface), trabecular bone, cortical bone, bone marrow, muscle, and usually
some active osteoblasts and osteoclasts (already remodelling the freshly formed
bone). Some of the slides include ends of two bones meeting at a synovial
joint, with endochondral ossification occurring in the ends of both long
bones.
The
slide labelled "developing cartilage bone" displays a longitudinal
section through the end of a long bone, at a fairly youthful stage in development
when only the shaft (diaphysis) has been mineralized and the end is still
cartilagenous. The slide illustrates the process of endochondral
ossification (in which cartilage is growing outward toward the end of
the bone, while bone tissue is following along behind, invading and replacing
the cartilage. In addition to endochondral ossification, you can of
course also see hyaline cartilage (the cartilage which faces the articular
surface), trabecular bone, cortical bone, bone marrow, muscle, and usually
some active osteoblasts and osteoclasts (already remodelling the freshly formed
bone). Some of the slides include ends of two bones meeting at a synovial
joint, with endochondral ossification occurring in the ends of both long
bones. The
slide labelled "fibrocartilage" displays considerably more
than fibrocartilage. It appears to be a section through the pubic symphysis,
with a more-or-less symmetrical arrangement of bone and muscle on either side
of the midline, with the bones bound together by a fibrocartilagenous joint
in the medial region of the preparation. Although collagen is present
in all cartilage, microscopically visible strands are only apparent in fibrocartilage,
where they contribute extra toughness. Active remodelling may be apparent in
the bone on this slide (as evidenced by the presence of active osteoblasts
and osteoclasts).
The
slide labelled "fibrocartilage" displays considerably more
than fibrocartilage. It appears to be a section through the pubic symphysis,
with a more-or-less symmetrical arrangement of bone and muscle on either side
of the midline, with the bones bound together by a fibrocartilagenous joint
in the medial region of the preparation. Although collagen is present
in all cartilage, microscopically visible strands are only apparent in fibrocartilage,
where they contribute extra toughness. Active remodelling may be apparent in
the bone on this slide (as evidenced by the presence of active osteoblasts
and osteoclasts). 
 Slides of "trachea" and "trachea and esophagus"
display the C-shaped
rings of cartilage that reinforce the trachea. Cartilage may also be
found in bronchial walls in the slide of "lung".
Slides of "trachea" and "trachea and esophagus"
display the C-shaped
rings of cartilage that reinforce the trachea. Cartilage may also be
found in bronchial walls in the slide of "lung". The
slides of "hyaline cartilage" and "elastic cartilage"
simply display examples of these two tissue types without much context. The
source for the hyaline cartilage is not obvious; the elastic cartilage example
may be from epiglottis (deducing from the appearance of the associated epithelium).
The elastic cartilage slide is stained for elastin (the fine purple
strands within the matrix); otherwise it would look just like hyaline cartilage.
Hyaline cartilage may be seen on several other slides, notably
"developing cartilage bone," "early dental cup," and "trachea."
The
slides of "hyaline cartilage" and "elastic cartilage"
simply display examples of these two tissue types without much context. The
source for the hyaline cartilage is not obvious; the elastic cartilage example
may be from epiglottis (deducing from the appearance of the associated epithelium).
The elastic cartilage slide is stained for elastin (the fine purple
strands within the matrix); otherwise it would look just like hyaline cartilage.
Hyaline cartilage may be seen on several other slides, notably
"developing cartilage bone," "early dental cup," and "trachea."
 The
slide labelled "early dental cup" displays many features
of facial development in a section across the snout of an unidentified animal
fetus. If you enjoy microscopy, figuring out this slide should be fun.
Symmetry about the midline should help you get oriented. You
can then find major anatomical features such as the tongue (with its texture
of crisscrossing muscle fibers), the nasal septum (hyaline cartilage), the
jaw, and various skull bones. You can then examine the appearance of
various bones in various stages of intramembranous or endochondral ossification.
You may also find developing muscles, teeth, salivary glands, and skin.
The
slide labelled "early dental cup" displays many features
of facial development in a section across the snout of an unidentified animal
fetus. If you enjoy microscopy, figuring out this slide should be fun.
Symmetry about the midline should help you get oriented. You
can then find major anatomical features such as the tongue (with its texture
of crisscrossing muscle fibers), the nasal septum (hyaline cartilage), the
jaw, and various skull bones. You can then examine the appearance of
various bones in various stages of intramembranous or endochondral ossification.
You may also find developing muscles, teeth, salivary glands, and skin.
 The
slide of "internal ear" displays the many elaborate structures
of the inner ear, all embedded in bone. This is also the only slide
we have in which some of bone has no obvious lamellar pattern, suggesting
it represents primary or woven bone that has not yet been replaced
by remodelling. If finding and seeing that sounds exciting to you, then
enjoy; but you should first become acquainted with the appearance of bone
in other specimens (listed above) which are not as complex.
The
slide of "internal ear" displays the many elaborate structures
of the inner ear, all embedded in bone. This is also the only slide
we have in which some of bone has no obvious lamellar pattern, suggesting
it represents primary or woven bone that has not yet been replaced
by remodelling. If finding and seeing that sounds exciting to you, then
enjoy; but you should first become acquainted with the appearance of bone
in other specimens (listed above) which are not as complex.


 Growth
occurs by two mechanisms.
Growth
occurs by two mechanisms.

 Changes
in the size and shape of bones during the period of growth imply some
bone reorganisation. Osteoblasts and osteoclasts constantly deposit
and remove bone to adjust its properties to growth-related demands on
size and/or changes of tensile and compressive forces.
Changes
in the size and shape of bones during the period of growth imply some
bone reorganisation. Osteoblasts and osteoclasts constantly deposit
and remove bone to adjust its properties to growth-related demands on
size and/or changes of tensile and compressive forces.