COMPONENTS of Connective Tissue
Connective tissue consists of cells embedded in an extracellular matrix.
The matrix, in turn, consists of fibers and ground substance.
Characteristic connective tissue cell types include both resident
cells and immigrant or wandering cells.
- Resident cells reside in the place where they are found:
- Immigrant cells travel about (typically in blood) and immigrate into particular locations:
TOP OF PAGE
Fibroblasts are the most common resident cells in ordinary connective
tissue. These are the cells responsible for secreting collagen
and other elements of the extracellular matrix. In so doing, fibroblasts
are essential for normal development and repair.
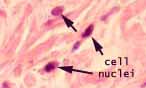
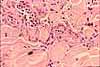
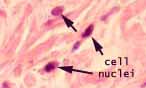 Throughout the body, fibroblasts all appear similar to one another. The nuclei of resting fibroblasts
appear dense (heterochromatic) and are usually flattened or spindle-shaped. Resting
fibroblasts typically have so little cytoplasm that the cells commonly appear,
by light microscopy, as "naked" nuclei. (In the thumbnail
image at right, the pink material is extracellular collagen.)
Throughout the body, fibroblasts all appear similar to one another. The nuclei of resting fibroblasts
appear dense (heterochromatic) and are usually flattened or spindle-shaped. Resting
fibroblasts typically have so little cytoplasm that the cells commonly appear,
by light microscopy, as "naked" nuclei. (In the thumbnail
image at right, the pink material is extracellular collagen.)
In microscopic appearance, even by electron microscopy, fibroblasts lack obvious specialized
features. "Nondescript" is perhaps the best word to describe the appearance of these cells in routine
histological specimens. There is little about fibroblasts
to attract the attention of a casual observer. Indeed, fibroblasts "are frequently overlooked as
'merely' ubiquitous supportive cells," to quote from a 2015 report in the journal Science
(https://www.science.org/doi/10.1126/science.aab0120).
Fibroblasts do more than just make collagen.
Significantly, each fibroblast knows
where in the body it resides and how it should contribute appropriately to the body's various connective tissues.
As reported in PLoS (28 July 2006),
individual fibroblasts express the genetic equivalent of a ZIP code: "Fibroblasts from different anatomic sites
have distinct and characteristic gene expression patterns" which are "systematically related to their positional
identities relative to major anatomic axes... For example, a cell on the hand expresses a set of genes that locate
the cell on the top half of the body (anterior) and another set of genes that locates the cell as being far away from
the body or distal and a third set of genes that identifies the cell on the outside of the body (not internal)."
This specificity of location is evident not only in the mechanical differences among various examples of loose and dense
connective tissues, such as tendon, ligament, and fascia, but most notably in the transparency
of the cornea of the eye.
Furthermore, signaling of positional awareness from fibroblasts can influence the differentiation of nearby tissues, such as
epidermis:
Clinical / research note (from Science, 5 Sept. 2024, Vol 385, pp. 1047-1048). "Differences between skin in different parts of the body are well recognized, but exploiting those differences to benefit the millions of people worldwide with prosthetic limbs is a new prospect. The skin of the palms and soles, known as volar skin, is specialized to withstand physical and mechanical forces, such as friction, shear stress, and pressure. Limb prostheses come into close contact with stump skin that is not adapted to these forces. As a result, the skin can break down, resulting in pain, ulceration, and infection... [Researchers demonstrated], in a clinical trial of healthy volunteers, that injecting autologous volar fibroblasts (derived from the volunteers' own tissue) confers volar features on nonvolar skin that persist for several months. This is a promising step toward improved quality of life for prosthesis wearers."
Indeed, the single cell type called "fibroblast" may properly represent
many distinctly (but invisibly) different cell types, such as "tendinocytes" (fibroblasts of tendons),
"keratocytes" (fibroblasts of cornea),
and "fasciacytes" (fibroblasts of fascia, so named in some texts, e.g., here). Undifferentiated
"mesenchymal stem cells," which retain a capacity for differentiation into other cell types
(see Science 324:1666, 26 June 2009)
may also be found within populations of fibroblasts.
For the role of fibroblasts in penile erection, see
Science 383 (9 Feb 2024), DOI: 10.1126/science.ade8064.
The name "fibroblast" itself is something of a misnomer,
since most cells with "blast" in their name are embryonic precursor
cells which subsequently differentiate into specialized cell types. Fibroblasts,
though, are already a mature, differentiated cell type (although some may retain the
capacity to differentiate into other mesenchymal cell types as well).
Fibroblasts are normally quiescent in mature tissues but become activated during
tissue repair following
injury. (Fibroblasts may also become activated during adaptive responses to mechanical stresses.)
When active, fibroblasts are manufacturing and secreting
collagen and other components of extracellular
matrix at the site of growth or tissue damage. Active fibroblasts appear larger than
resting ones, with more cytoplasm and with nuclei that are more euchromatic
(less densely stained); some texts refer to active fibroblasts as fibrocytes.
Scar formation: Resting fibroblasts retain the ability to become
active and to multiply when necessary, as during healing after injury. Scars
are formed by fibroblast activity during tissue repair. The substance
of the scar is collagen deposited by fibroblasts to
replace damaged tissue.
For an image of scar formation, see WebPath.
For recent research on fibroblast involvement in scar formation, see Science (17 April 2015) and Science (23 April 2021).
Closely related to fibroblasts are the chondroblasts which produce
the matrix of cartilage and the osteoblasts
which produce the matrix of bone.
Terminology: The appearance of "blast"
in a cell name normally indicates an embryonic cell that transforms
into a mature cell type (e.g., neuroblast, myoblast). However, in
the case of "fibroblast," "chondroblast," and "osteoblast,"
this designation indicates a cell which secretes fibers, cartilage
or bone.
TOP OF PAGE
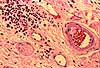
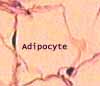
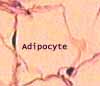
Adipocytes. Adipocytes are large connective tissue cells which
contain a substantial amount of lipid stored in the form of conspicuous round
droplets. Adipocytes function primarily as warehouses for reserve energy.
They also have endocrine function, secreting the hormone leptin to regulate hunger.
En masse hypodermal adipocytes can also assist in thermoregulation (maintaining body
temperature) by providing some insulation. In a few sites adipocytes also offer some
cushioning capacity (e.g., around kidneys, behind eyeballs).
Since most loose connective tissue contains scattered clusters
of adipocytes, the term adipose tissue is usually reserved for large
masses (grossly visible) of these cells.
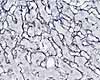
The most common type of adipocyte is called the unilocular adipocyte
or white fat. Each cell contains one single fat droplet (hence,
unilocular) surrounded by a thin rim of cytoplasm.
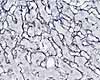
 Under
the light microscope, the appearance of an adipocyte is that of a conspicuous
clear space with a very thin border. The lipid droplet which comprises
the bulk of each adipocytes is not stained by ordinary aqueous stains, and
may even be removed by solvents during specimen preparation. Furthermore,
adipocyte cytoplasm itself is inconspicuously thin, and the nucleus of any
particular adipocyte is unlikely to be included in any given section (see
Viewing Tissues).
Under
the light microscope, the appearance of an adipocyte is that of a conspicuous
clear space with a very thin border. The lipid droplet which comprises
the bulk of each adipocytes is not stained by ordinary aqueous stains, and
may even be removed by solvents during specimen preparation. Furthermore,
adipocyte cytoplasm itself is inconspicuously thin, and the nucleus of any
particular adipocyte is unlikely to be included in any given section (see
Viewing Tissues).
On microscope slides, clusters of adipocytes present an
appearance somewhat like a "foam." The individual "bubbles,"
each representing a lipid droplet within a single cell, are fairly consistent
in size. Typical fat cell diameter is about 50 micrometers, comparable
to a skeletal muscle fiber or a small (terminal) arteriole.
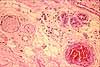
 The
shape of the droplet, in a tissue section on a slide, depends on how carefully
the specimen was prepared. Ideally the droplets are smooth and round
(as in the image above), but they may also be distorted, shaped more like
jigsaw-puzzle pieces (as in the image at right).
The
shape of the droplet, in a tissue section on a slide, depends on how carefully
the specimen was prepared. Ideally the droplets are smooth and round
(as in the image above), but they may also be distorted, shaped more like
jigsaw-puzzle pieces (as in the image at right).
Adipocytes may occur in almost any sample of ordinary connective
tissue, where they may be found as individual cells or in clumps. Even
when clustered together and apparently touching, adipocytes remain separated
by a thin layer of matrix (ground substance and collagen) which includes
numerous capillaries.
A layer of adipose tissue in the deep layers of skin (variously
called hypodermis or subcutaneous adipose) may provide significant
thermal insulation.
A more specialized and localized type of adipocyte
is called the multilocular adipocyte or brown fat. These
cells function in thermogeneration, essentially burning fat to produce heat.

 Individual brown fat cells contain numerous small lipid droplets (hence the name multilocular)
and numerous mitochondria (whose cytochromes confer a brownish color to unstained brown fat). In
these cells, the metabolic reactions of the mitochondria are uncoupled from
ATP synthesis so that energy produced is simply released as heat.
Individual brown fat cells contain numerous small lipid droplets (hence the name multilocular)
and numerous mitochondria (whose cytochromes confer a brownish color to unstained brown fat). In
these cells, the metabolic reactions of the mitochondria are uncoupled from
ATP synthesis so that energy produced is simply released as heat.
Infants have a substantial amount of brown fat, especially
in a pad between the shoulder blades. Brown fat is scarce in adults
but may be found around the adrenal gland. Recent research (three
articles in New England Journal of Medicine 360[15], 9 April 2009)
reported brown fat in a region extending from the anterior neck to the thorax;
brown fat activity was positively related to resting metabolic rate and
was significantly lower in overweight or obese subjects than in lean subjects.
TOP OF PAGE
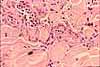
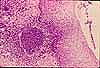
Macrophages remove and digest the by-products of both bacterial
warfare and normal growth and degeneration. Resting macrophages are
difficult to recognize reliably by light microscopy, at least in routine preparations,
because they lack conspicuous distinguishing characteristics. They tend
to be somewhat larger than fibroblasts, with more cytoplasm. Macrophages
contain numerous lysosomes which are used for breaking down ingested material.
These lysosomes are usually inconspicuous by light microscopy but readily
visible by electron microscopy.
 In macrophages which have been active and have accumulated indigestible residue,
the lysosomes may be visible by light microscopy as brown intracellular
granules, as in this image of lung macrophages ("dust cells").
Click here or on the image for a wider-field
view and more information on lung macrophages.
In macrophages which have been active and have accumulated indigestible residue,
the lysosomes may be visible by light microscopy as brown intracellular
granules, as in this image of lung macrophages ("dust cells").
Click here or on the image for a wider-field
view and more information on lung macrophages.
Historical notes: Macrophages
of liver (Kupffer cells) and of lung
(dust cells) were named prior to clear understanding that these cells belong
to a more widely distributed cell type.
The obsolete term reticuloendothelial system refers
to the macrophages of the liver, spleen
and lymph nodes (i.e., those organs
with elaborate endothelially-lined channels supported by reticular
connective tissue). The name reflects former confusion about the
distinction between endothelial cells and the scattered population of macrophages
(monocytes, histiocytes). Macrophages can be readily labelled experimentally
through their phagocytosis of injected carbon particles. However,
endothelial cells are also labelled by the same procedure. Although
endothelial cells are not dramatically phagocytotic, they do shuttle some
materials across the endothelial lining via small endocytotic and exocytotic
vesicles.
Macrophages are mobile (amoeboid movement) over short distances within a
local region of connective tissue. Most ordinary connective tissue contains
a standing population of resident macrophages. But when damage or infection
requires reinforcements, monocytes can increase
the macrophage population many-fold. Monocytes are circulating cells
in the blood which can differentiate into macrophages when they enter connective tissue.
Macrophages are among the most independent cells
in the body. Although they respond to the chemical signals which govern
immune responses, individual macrophages are capable of crawling out of
connective tissue, crossing the body's epithelium, and scavenging foreign
material on exposed surfaces such as the alveolar lining of the lung and
the conjunctiva of the eye.
Macrophages attempt to engulf foreign material by gathering together and merging into foreign body giant cells
(see Webpath).
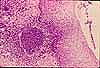
Those associated with granulomas (Webpath) are called
Langhans giant cells (commemorating Theodor Langhans, b. 1839).
TOP OF PAGE
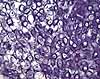
Mast cells are secretory alarm cells. Upon the slightest disturbance,
they release chemical signals which diffuse through the surrounding ground
substance and trigger the process of inflammation.
Mast cells occur as small individual cells, scattered rather widely in ordinary
connective tissue. The cytoplasm of mast cells is packed with secretory
vesicles, which can be fairly conspicuous in high-quality light microscope
preparations. The granules contain histamine, heparin, and various
other chemical mediators whose release signals a number of physiological defense
responses.
Allergies are caused (in part) by inappropriate sensitivity
of mast cells. The symptoms are treated with antihistamines,
chemicals which interfere with the action of histamine.
Historical note. The name "mast cell"
is a misnomer. The word "mast" refers to food. When
first described, the secretory vesicles of mast cells were misinterpreted
as evidence of ingestion by phagocytosis. So the name suggests a cell
which has eaten its fill of "mast."
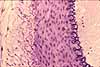
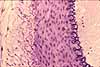
 Lymphocytes are principal
elements of the immune system. They
are small cells with round nuclei and minimal cytoplasm (the example shown
here is from a blood smear). Some lymphocytes circulate throughout the
body, moving freely from blood to ordinary connective tissue and back again.
[Recent research suggests that some types of lymphocytes are more compartmentalized.]
Lymphocytes serve both as scouts and as weapons against invading microorganisms.
Lymphocytes are principal
elements of the immune system. They
are small cells with round nuclei and minimal cytoplasm (the example shown
here is from a blood smear). Some lymphocytes circulate throughout the
body, moving freely from blood to ordinary connective tissue and back again.
[Recent research suggests that some types of lymphocytes are more compartmentalized.]
Lymphocytes serve both as scouts and as weapons against invading microorganisms.
 Lymphocytes occur as inconspicuous individual cells scattered through most ordinary
connective tissues. They are especially common in lamina propria
(i.e., the connective tissues of mucous membranes). Microscopically conspicuous
accumulations of lymphocytes occur in scattered sites around the body, with
special concentrations in spleen,
thymus, lymph
nodes, Peyer's patches of ileum,
and tonsils. These sites include
germinal centers where activated lymphocytes proliferate.
Lymphocytes occur as inconspicuous individual cells scattered through most ordinary
connective tissues. They are especially common in lamina propria
(i.e., the connective tissues of mucous membranes). Microscopically conspicuous
accumulations of lymphocytes occur in scattered sites around the body, with
special concentrations in spleen,
thymus, lymph
nodes, Peyer's patches of ileum,
and tonsils. These sites include
germinal centers where activated lymphocytes proliferate.
Lymphocytes manufacture antibodies, proteins which possess the ability to
recognize and bind to foreign substances. The antibodies may be either
secreted or bound to the lymphocyte membrane. Plasma cells are
differentiated lymphocytes which are specialized to manufacture and secrete
relatively large amounts of antibody.
[More on lymphocytes in inflammation.]
Other connective tissue cell types. The list above is not exhaustive.
TOP OF PAGE
EXTRACELLULAR MATRIX
The extracellular matrix of connective tissue is composed of fibers and
ground substance. In ordinary connective
tissue, the principal fiber type is collagen (the most
abundant protein in the body), with elastic fibers
as a minor element; ground substance consists mainly of water.
This matrix is considerably more complex than described below. For a readable review of this complexity, including
its interactions with associated cells, see
Science vol. 369, p. 659 (2023).
Ground substance is the background material within which all other
connective tissue elements are embedded. In ordinary connective tissue,
the ground substance consists mainly of water whose major role is to provide
a route for communication and transport (by diffusion) between tissues. This
water is stabilized by a complex of glycosaminoglycans (GAGs), proteoglycans,
and glycoproteins, all of which comprise only a small fraction of the
weight of the ground substance.
The effect of GAGs in water is quite like that of Jello™.
If you've ever made Jello™, you know that a couple tablespoons
of powder from the Jello™ package can turn a quart or more of water
from a flowing liquid into a solid mass.
Ground substance may be highly modified in the special
forms of connective tissue.
- In blood, the ground substance lacks stabilizing macromolecules.
We call this free-flowing ground substance plasma.
- In skeletal tissue,
the ground substance may become mineralized by deposition of calcium salts.
We call this rigid ground substance bone.
- In cartilage,
the ground substance is much more solid than in ordinary connective tissue
but still retains more resiliency than bone.
The extracellular fibers of connective tissue are traditionally classified
into three types:
Collagen is the most common protein in the body. As an essential
structural element in the extracellular matrix of
most connective tissues, including bone and cartilage, collagen confers
toughness and tensile strength. Scars are made
of collagen.
More than a dozen different varieties of collagen exist
in the body, usually identified by Roman numerals. These varieties
are produced by different genes, have somewhat different properties, and
occur in different locations. The most common forms are listed below.
 The type I collagen fibers of ordinary fibrous connective tissue are colorless,
so in most cases their bulk appearance is white (e.g., the "white"
of the eye and other organ sheaths, of tendons, and of fascia). Whiteness results
from scattering of light (the same reason that snow is white, even though
snowflakes are transparent crystalline ice). Under extraordinary circumstances
of regular fiber arrangement and controlled extracellular fluid, as in the
cornea of the eye, bulk
collagen can be transparent.
The type I collagen fibers of ordinary fibrous connective tissue are colorless,
so in most cases their bulk appearance is white (e.g., the "white"
of the eye and other organ sheaths, of tendons, and of fascia). Whiteness results
from scattering of light (the same reason that snow is white, even though
snowflakes are transparent crystalline ice). Under extraordinary circumstances
of regular fiber arrangement and controlled extracellular fluid, as in the
cornea of the eye, bulk
collagen can be transparent.
 Although colorless, type I collagen is eosinophilic and so appears pink in
routine H&E stained tissue specimens.
Such pink collagen fibers are the most prominent feature of ordinary
connective tissue. The ability to locate and identify connective tissue
on slides is largely the ability to recognize collagen fibers. (Collagen can be selectively stained with
trichrome stains, to help distinguish it from other eosinophilic fibers
like smooth muscle.)
Although colorless, type I collagen is eosinophilic and so appears pink in
routine H&E stained tissue specimens.
Such pink collagen fibers are the most prominent feature of ordinary
connective tissue. The ability to locate and identify connective tissue
on slides is largely the ability to recognize collagen fibers. (Collagen can be selectively stained with
trichrome stains, to help distinguish it from other eosinophilic fibers
like smooth muscle.)
Collagen is produced by fibroblasts.
Fibroblasts secrete procollagen molecules, which are converted extracellularly
into tropocollagen. Tropocollagen then self-assembles into microscopically
visible fibers and grossly evident mechanical structures such as tendons.
(For further introduction to the biochemistry and related pathology of collagen
synthesis, see Kierszenbaum, Histology and Cell Biology, or follow this
link to the NIH NLM.)
The assembly of collagen into anatomical features seems almost magical, since
the process takes place in extracellular space, presumably guided (somehow)
by fibroblasts. This "magic" is perhaps most evident
in the cornea of the eye. In routine histological
preparations, the cornea is almost indistiguishable from the sclera.
Both consist of densely-packed collagen fibers. But whereas the sclera (the "white" of the eye) is opaque,
the cornea is marvellously transparent. In the cornea, collagen fibers
are arranged into an almost crystalline array of extremely regular layers, with fiber
orientation parallel within each layer but alternating between adjacent layers.
(Activity of corneal endothelial cells is also essential to maintain the appropriate
fluid balance for transparency

Reticular fibers (rete, net), made from type III collagen, provide a very
delicate network (hence the name) supporting individual cells in certain organs
(lymph nodes, spleen,
liver). Reticular fibers do not show
up in routine H&E stained specimens,
but they can be demonstrated with silver salts.
The collagen which reinforces cartilage, bone, basement
membranes, basal lamina, and assorted other structures is not organized
into microscopically visible fibers.
 Elastin is another fibrous protein. As the name suggests, elastin is elastic.
In ordinary connective tissue, elastic fibers help restore normal shape
after distortion. In high enough concentrations, elastin confers a yellowish
color (as in the elastic ligament, ligamentum flavum, where flavum
= yellow)
Elastin is another fibrous protein. As the name suggests, elastin is elastic.
In ordinary connective tissue, elastic fibers help restore normal shape
after distortion. In high enough concentrations, elastin confers a yellowish
color (as in the elastic ligament, ligamentum flavum, where flavum
= yellow)
Like rubber bands, elastic fibers can deteriorate with
age and exposure to sun. This effect is easily demonstrated by recruiting
two volunteers, one youthful and one elderly. Pinch up a bit of skin
on the back of each person's hand and then watch how quickly the skin returns
to its original position when released.
 In
elastic ligaments, dense elastic fiber concentrations convey strong elastic
properties while a lesser concentration of collagen serves simply as a mechanical
stop to prevent over-stretching under severe stress.
In
elastic ligaments, dense elastic fiber concentrations convey strong elastic
properties while a lesser concentration of collagen serves simply as a mechanical
stop to prevent over-stretching under severe stress.
 In
addition to its occurrence as a minor constituent in most ordinary connective
tissue, elastin is also characteristic of arterial
walls (especially elastic arteries such as the aorta) and of
elastic cartilage (found in
ear and epiglottis).
In
addition to its occurrence as a minor constituent in most ordinary connective
tissue, elastin is also characteristic of arterial
walls (especially elastic arteries such as the aorta) and of
elastic cartilage (found in
ear and epiglottis).
Elastic fibers are often poorly stained by H&E,
and so are seen microscopically only with specially stained slides.
TYPES of Connective Tissue
Like everything else, connective tissues can be descriptively sorted into various types.
The standard descriptive scheme is based on the relative proportions of various cellular and
extracellular components.
This scheme is not altogether satisfactory, since the proportion of each component can
vary along its own continuum. And it is helpful to remember that all types of connective
tissue share a fundamental commonality of cellular and matrix components.
"Ordinary" connective tissue
is a generalized form of connective tissue which contains all of the basic
components of connective tissue in reasonable proportion, including cells
(of several types), extracellular fibers, and extracellular
ground substance. Loose ordinary connective tissue
is sometimes called areolar tissue. Variations in the relative proportions
and arrangements of cells, fibers, and ground substance are used to describe/classify
various more-specialized types of connective tissues.
"Special" connective tissue. Within a background texture of
rather universally distributed ordinary connective tissue, there also occur
several very highly differentiated and localized forms of "special" connective
tissue, which nevertheless share many common features (structural components,
cell lineages) with connective tissue proper. These special forms
include bone, cartilage,
lymphoid tissue (spleen and lymph nodes),
blood, and bone marrow.
In routine use, the term "connective tissue" usually refers
to ordinary connective tissue, while the special forms are more commonly referred
to by their specific names (e.g., bone, cartilage, blood).
TOP OF PAGE
Loose / Dense. Connective tissue may be distinguished as either
loose or dense, depending on the proportion of fibers. The intrinsic strength of
collagen is the same in both loose and dense connective
tissue.
Loose and dense are not two different kinds of connective tissue, but rather descriptors
for a continuous range of variation in looseness / denseness.
The difference between moderately loose connective tissue and moderately
dense connective tissue is difficult to appreciate by microscopy, since inadvertent
compression or stretching may reduce or exaggerate the space between the fibers.
This difference is better appreciated at the level of gross anatomy.
If a fresh sample of loose connective were hit with
a hammer, it would "squish." If a sample of really dense
connective tissue, such as tendon, were hit, the hammer would bounce back.
But there is no sharp distinction between loose and dense connective tissue;
the labels refer to the extremes of a continuum.
Dense connective tissue is so named because of
high density of extracellular fibers, and relatively
smaller proportions of ground substance and cells.
Densely packed type I collagen fibers provide main strength
with resistance to tearing and stretching.
 Dense collagenous connective tissue is found wherever the tensile strength
of collagen is of paramount importance. Examples
include dermis (the layer of the skin
which yields leather), tendons and ligaments,
and organ sheaths (such as the "white" of the eye (sclera),
the cornea, or the capsule of the kidney).
Dense collagenous connective tissue is found wherever the tensile strength
of collagen is of paramount importance. Examples
include dermis (the layer of the skin
which yields leather), tendons and ligaments,
and organ sheaths (such as the "white" of the eye (sclera),
the cornea, or the capsule of the kidney).
Dense elastic connective tissue is found wherever
the elasticity of elastin is of paramount importance,
as in the ligamentum flavum (flavum refers to the yellow
color conferred by the elastin) and the aorta.
Loose connective tissue has
a relatively large proportion of ground substance,
of cells, or of both cells and ground substance. In
other words, loose connective tissue lacks the massive fibrous reinforcement
that characterizes dense connective tissue. Nevertheless, the same
types of fibers are still found, although fewer and
more delicate.
 Fluid may be able to move fairly freely through loose connective tissue.
Bruising ("ecchymosis") can display
evidence of such movement.
Fluid may be able to move fairly freely through loose connective tissue.
Bruising ("ecchymosis") can display
evidence of such movement.
Loose connective tissue is easily distorted, permitting
tissues on either side to move freely with respect to one another. However,
when loose connective tissue is distorted sufficiently, it too becomes
tough and resists further deformation.
Loosely packed collagen
fibers (in tissues such as hypodermis
or the submucosa of internal organs) allow free movement within definite
limits.
Do-it-yourself demonstration: To experience the mechanical
quality of loose connective tissue, try the following. (1) Pinch
the skin of one cheek between thumb and forefinger. (2) Hold the
lining (mucosa) of that cheek between your teeth. (3) Then move
the skin relative to the lining. See how far the two surfaces can
move relative to one another. The freedom is due to the looseness
of the intervening connective tissue. The limits are set by the
collagen fibers which become straightened until
taut.
Ordinary loose connective tissue, sometimes called areolar tissue,
is common throughout the body. (The word areolar
refers to areolar tissue's variable spaces (areolae) filled with ground substance.) Examples
of areolar tissue include hypodermis,
lamina propria, submucosa,
mesentery, and fascia.
(Fascia [L., band] is the term used in gross anatomy for
the connective tissue that loosely binds together various other structures.)
TOP OF PAGE
Regular/Irregular. Dense connective
tissue may be further described as either regular or irregular,
depending on the orientation of the fibers.
In regular connective tissue (example: tendon)
the fibers are all aligned in a single direction,
conferring tensile strength primarily in that direction.
In irregular connective tissue (example: dermis)
the fibers are arranged in various directions,
although even here collagen fibers may adopt a preferential orientation
as revealed by "Langer's lines."
 Fibrocollagenous
(or just fibrous) tissue contains a substantial proportion of
collagen. A principal feature of fibrous tissue
is flexibility combined with great tensile strength.
Fibrocollagenous
(or just fibrous) tissue contains a substantial proportion of
collagen. A principal feature of fibrous tissue
is flexibility combined with great tensile strength.
Because collagen is colorless and typically scatters light,
fibrous connective tissue usually appears white.

The sclera (or "white") of the eye is
a readily visible example of dense fibrous connective tissue comprising
an organ sheath.
Tendons and muscle capsules may also be familiar
from the butcher shop or anatomy lab. The ends of muscle
fibers are typically attached to dense fibrous connective tissue of
periosteum, tendon, or ligament.
The dermis of the skin
is also fibrous connective tissue (hence, leather is mostly collagen).
Elastic tissue is a dense connective tissue which contains predominantly
elastic fibers rather than collagen. It is more
elastic (obviously) than dense collagenous connective tissue.
Examples include the wall of the aorta and the elastic
ligament of the spine (called ligamentum flavum [flavum =
yellow] because in sufficient quantity elastin is yellowish).
 Adipose
tissue is loose connective tissue which is dominated by fat
cells, or adipocytes. Since most loose
connective tissue contains scattered clusters of adipocytes,
the term adipose tissue is usually reserved for large masses (grossly
visible) of these cells.
Adipose
tissue is loose connective tissue which is dominated by fat
cells, or adipocytes. Since most loose
connective tissue contains scattered clusters of adipocytes,
the term adipose tissue is usually reserved for large masses (grossly
visible) of these cells.
 Lymphoid
tissue is loose connective tissue with large numbers of lymphocytes
that have accumulated in the tissue. Lamina
propria (the loose connective tissue of mucosal surfaces) often shows
lymphatic tendencies, or even fairly well-developed lymph nodules. The
immune cells in these locations form a vital second line of defense (the epithelium
with its continuous but rather easily broken wall was the first line) against
invading microorganisms.
Lymphoid
tissue is loose connective tissue with large numbers of lymphocytes
that have accumulated in the tissue. Lamina
propria (the loose connective tissue of mucosal surfaces) often shows
lymphatic tendencies, or even fairly well-developed lymph nodules. The
immune cells in these locations form a vital second line of defense (the epithelium
with its continuous but rather easily broken wall was the first line) against
invading microorganisms.
A separate page describes the lymphatic
system, including lymphoid tissues in several specialized lymphoid organs
-- spleen, thymus,
lymph nodes, and tonsils.
Lymphoid organs are also sometimes called reticular tissue because of
the supporting framework of reticular fibers (a delicate,
branching form of collagen).
TOP OF PAGE
Areolar tissue is another name for loose irregular
connective tissue, with unspecialized proportions of the various matrix
components and cells. The word "areolar" in its name refers to the many small spaces (areolae),
of variable size and filled with ground substance, that characterize this tissue.
Examples of areolar tissue occur
throughout the body.
Historical note: Among the 21 simple tissues described by
Bichat in 1801, areolar tissue occupies first place (Bichat's 1° tissu le cellulaire).
Bichat recognized the significance of areolar tissue in the spread and/or limitation of inflammatory processes.

For a fascinating essay on the "discovery" of areolar tissue, see
Forrester: "The homoeomerous parts and their replacement by Bichat's tissues," in
Medical History, 1994, 38: 444-458,
especially pp. 452-454.
Although areolar tissue may be seen on many slides, slide sets commonly include a whole-mount
preparation of mesentery which is
labelled as "Areolar Tissue."
Blood is traditionally classified as a specialized
form of connective tissue, with no fibers, highly fluid ground substance,
and mobile cells. Blood is thus distinct from ordinary connective tissue.
However, blood may also be usefully regarded as simply a fraction of
ordinary connective tissue that is free to gallop around from place to place
along differentiated highways. (Follow the links for a more extensive
discussion of blood.)
Only the red blood cells,
like trolley cars, are confined to the highways (i.e., blood vessels). All
other cell types in blood, and most plasma constituents as well, can circulate
rather freely from blood to connective tissue and back again. Thus,
most of the mobile cellular components of ordinary connective tissue are
interchangeable with those in blood.
Cell names may differ between blood and ordinary connective
tissue. The cells which are called macrophages
in ordinary connective tissue are called monocytes
in blood. Blood cells similar to tissue mast
cells are called basophils.
From this point of view, the term "white
blood cell" is not only very nonspecific but is also a misnomer. "Circulating
connective tissue cell" (still nonspecific) better fits the functional location
of these mobile cell types.
Bone and cartilage
are special forms of connective tissue, made by specialized osteoblasts and
chondroblasts, with uniquely solidified ground substance. These forms
are described on a separate page, as skeletal
tissue.
FUNCTIONS of Connective Tissue
Most connective tissue is serving several vital functions simultaneously,
including --
After injury, connective tissue is instrumental in tissue repair,
specifically in scar formation.
Additional functions found in specialized sites include --
Transport
The circulatory system is the familiar mechanism for moving materials around
the body. However, blood vessels do not go quite far enough. Most
cells are not situated directly against capillaries, but rather some tens
or even hundreds of micrometers (several cell diameters) away from the nearest
blood vessel.
Connective tissue (more specifically the stabilized water
in the ground substance) provides the final pathway for diffusion of nutrients,
oxygen, waste and metabolites to and from the cells of the body.
Subcutaneous and intramuscular injection of drugs also
makes use of connective tissue as the initial transport medium.
All blood vessels are embedded in connective tissue. The only cells
which receive their sustenance directly from the blood are the endothelial
cells lining the vessels themselves. All other cells are supplied via
diffusion through intermediary connective tissue.
The transport functions of blood and connective tissue
cannot be separated. In essence, blood is
really just a mobile fraction of connective tissue. The heart and
circulatory system simply facilitate the movement of this traveling tissue.
Whenever you find elaborate capillary beds closely associated
with groups of cells (such as the capillary networks enveloping skeletal
muscle fibers or encircling secretory acini), you can predict that these
cells must have some exceptionally high demand for transport in or out,
since a resting cell can live quite happily at some distance from the nearest
blood supply. Rich capillary supply is characteristic of muscle and
brain (supplying oxygen), lung (acquiring oxygen), intestinal villi (collecting
nutrients), exocrine glands (delivering raw materials for secretion), and
endocrine glands (collecting hormones).
Immunological surveillance and defense
Connective tissue serves not only as a transportation route for the body's
normal economy but also as a convenient route for invading microorganisms. To provide defense
against this eventuality, an army of various cell types is deployed throughout
the connective tissue.
Bacteria do not easily proliferate within epithelia -- cell
membranes block entry into cells, and there is little extracellular food
for bacteria within epithelia. On the other hand, connective tissue
offers a potential paradise. The abundant extracellular material provides
all the necessary nutrients as well as an ideal warm, humid, oxygenated
environment. Without vigorous immunological defenses within the connective
tissue, any small break in the epithelium would convert the body into an
excellent bacterial culture.
Immunological defense engages a process called inflammation.
Inflammation is a specific function
of connective tissue.
Ordinary connective tissue includes two resident cell types with immunological
function, mast cells and macrophages.
(Resident cells, which essentially remain fixed in place waiting
for action, are distinguished from wandering or immigrant cells
which migrate in and out of the tissue.)
Mast cells
are secretory alarm cells. They are very fragile, rupturing at any
disturbance. The release of their granules (stored secretory product)
triggers a number of physiological defense mechanisms, including inflammation.
Macrophages remove and digest
the by-products of both bacterial warfare and normal growth and degeneration.
Monocytes, which are circulating cells in the blood, differentiate
into macrophages when they enter connective tissue. Macrophages are
mobile (amoeboid movement) over short distances within a local region of
connective tissue. But when an invasion requires reinforcements, immigrating
monocytes can increase the macrophage population many-fold.
Other fixed cells (i.e., fibroblasts
and fat cells) are primarily structural, although
fibroblast activity (cell proliferation and secretion of collagen)
is an important aspect of the healing process.
Ordinary connective tissue also includes several wandering cell types, also called
white blood cells, which travel in and out of connective tissue. Five basic
types may be considered (follow the links for each cell type, for much more detail):
- Lymphocytes
circulate through both blood and connective tissue. They possess in
their secretory product and on their cell membranes the ability to recognize
and bind to foreign substances.
 Neutrophils (properly, neutrophilic granulocytes) take their name from the staining
properties, neither acidophilic nor basophilic, of these cells' specific
granules. Neutrophils travel in blood until called out
into peripheral tissues. An inflammatory response
(triggered in part by mast cells) summons neutrophils
to the affected area. Neutrophils have the ability to approach, engulf,
and kill most bacteria.
Neutrophils (properly, neutrophilic granulocytes) take their name from the staining
properties, neither acidophilic nor basophilic, of these cells' specific
granules. Neutrophils travel in blood until called out
into peripheral tissues. An inflammatory response
(triggered in part by mast cells) summons neutrophils
to the affected area. Neutrophils have the ability to approach, engulf,
and kill most bacteria. - Eosinophils, like
neutrophils, are named according to their characteristic staining; their
cytoplasmic granules are eosinophilic. Eosinophils
are involved in responses to allergy and parasites.
- Basophils, like neutrophils
and eosinophils, are named according to their characteristic staining. Their
cytoplasmic granules are basophilic. Basophils
are the circulating equivalent of tissue mast cells.
- Monocytes are circulating
precursors of macrophages.
The distribution of the wandering immune cells reflects ongoing physiological
and pathological processes.
- Neutrophils
are normally confined to circulating blood, where they remain ready for
defensive reactions. A gathering of neutrophils (polymorphonuclear
neutrophilic leukocytes, or PMNs) outside of blood signifies an acute inflammation,
with tissue damage and/or presence of infectious microorganisms.
- Lymphocytes accumulate later
and may indicate chronic inflammation. In
some regions (as in tonsils and
in lamina propria along the
gut), accumulations of lymphocytes are part
of a normal (nonpathological) interaction with antigens (foreign materials)
which cross the epithelium.
For more about the immune system, see CRR
Lymphatic System.
TOP OF PAGE
Mechanical Support
The mechanical quality of most ordinary connective tissue is affected only
indirectly by the cells which occur within it (unlike epithelial
tissue, which consists entirely of cells).
An exception is adipose tissue,
where the sheer bulk of many adipocytes can offer
mechanical protection by cushioning impact.
The major determinant of the mechanical properties of most connective tissue
is the extracellular matrix which is secreted by the
cells within it (fibroblasts in ordinary connective
tissue, osteoblasts and chondroblasts
in bone and cartilage respectively).
In ordinary connective tissue, the ground substance
is too fluid to provide much strength. The jelly-like ground substance
of ordinary connective tissue serves mainly to prevent extracellular water
from pooling in the lowest part of your body. But ground
substance can be a major structural feature in special forms such as cartilage
and bone.
In most connective tissue, extracellular fibers form
the main structural elements.
Collagen offers flexibility with high tensile strength.
Densely packed collagen fibers provide strength with resistance to
tearing and stretching. Loosely packed collagen fibers allow free
movement within definite limits.
Reticular fibers (really, a special form of collagen)
provide a delicate supporting framework for individual cells, especially
when such cells accumulate en masse to form a large solid organ such as
the spleen or the liver.
Elastin, as the name suggests, is stretchy like
rubber bands, helping restore normal shape after distortion. In elastic
ligaments and arteries dense elastic fiber concentrations convey strong
elastic properties while a lesser concentration of collagen serves simply
as a mechanical stop to prevent over-stretching under severe stress.
Growth and Repair. The most common fixed cell of ordinary connective
tissue proper is the fibroblast. Fibroblasts
are normally quiescent in the adult. During growth and also during repair
after injury fibroblasts are active secretory cells which manufacture the
fibers and ground substance of
connective tissue. They also retain the ability to multiply when necessary,
as during wound healing, and possibly to differentiate into other mesenchymally
derived cell types (such as vascular endothelium
and smooth muscle). Myofibroblasts resemble fibroblasts but have an
additional contractile ability, useful for example for closing wounds.
A scar is collagen deposited by fibroblasts during repair.
According to recent research, genetically differentiated
fibroblasts may also be responsible for guiding localized patterns of tissue
organization during growth and repair.
Energy Economics. Connective tissue is involved in several interrelated
ways with energy storage and thermoregulation.
The burden of reserve energy storage falls almost entirely on adipocytes.
Many other cells, especially muscle cells, have short-term
energy stores in the form of intracellular glycogen. A larger, but
still comparatively small, energy reserve is also provided by glycogen in
hepatocytes (the epithelial cells
of liver). But adipocytes
exceed all other cell types for calories stored per cell.
Accumulations of subcutaneous fat cells also provide
thermal insulation. And specialized brown
fat (also called multilocular fat) is responsible for generating heat
to maintain body temperature under circumstances when insulation is not sufficient.
This heat-producing function is especially significant for infants (and
other small mammals) and may be related to metabolic rate in adult humans.
Haemopoiesis, the process of blood cell formation, also falls
to connective tissue. In the adult, haemopoiesis takes place in the connective
tissue of bone marrow. Bone marrow is
specialized for this role. (Pass over this lightly now.
You should learn more in Year Two.)
 TYPES
of connective tissue
TYPES
of connective tissue

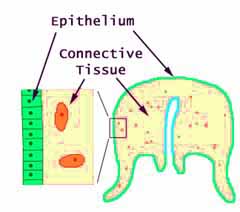 The location of connective
tissue relative to other tissues may be easily understood in a simple animal
like a jellyfish.
The location of connective
tissue relative to other tissues may be easily understood in a simple animal
like a jellyfish.




 The
shape of the droplet, in a tissue section on a slide, depends on how carefully
the specimen was prepared. Ideally the droplets are smooth and round
(as in the image above), but they may also be distorted, shaped more like
jigsaw-puzzle pieces (as in the image at right).
The
shape of the droplet, in a tissue section on a slide, depends on how carefully
the specimen was prepared. Ideally the droplets are smooth and round
(as in the image above), but they may also be distorted, shaped more like
jigsaw-puzzle pieces (as in the image at right).