Histology Topics for Lincoln Scholars Program
CAVEAT: As they say, all rules have exceptions. The account on this page should be regarded as a broad-brush overview, a caricature which captures some essential architecture of most organs but simplifies or elides many details that can be easily appreciated later, with further study of particular organs. Take "always" and "everywhere" with a grain of salt.
(The phrase "with a grain of salt" actually has a medical origin, attributed to Pliny the Elder regarding antidotes to poison.)
 |
Esophageal mucosa |
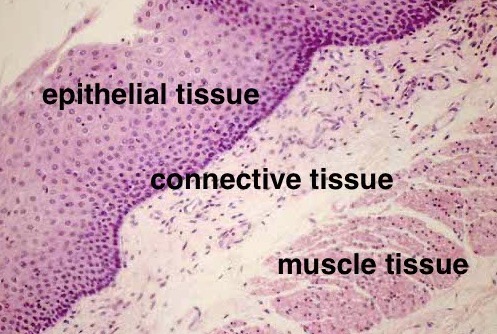
These relationships hold true throughout the body, so that connective tissue can be found practically everywhere, along with the muscles, nerves, and vessels that lie within it and the epithelium which lies upon it.
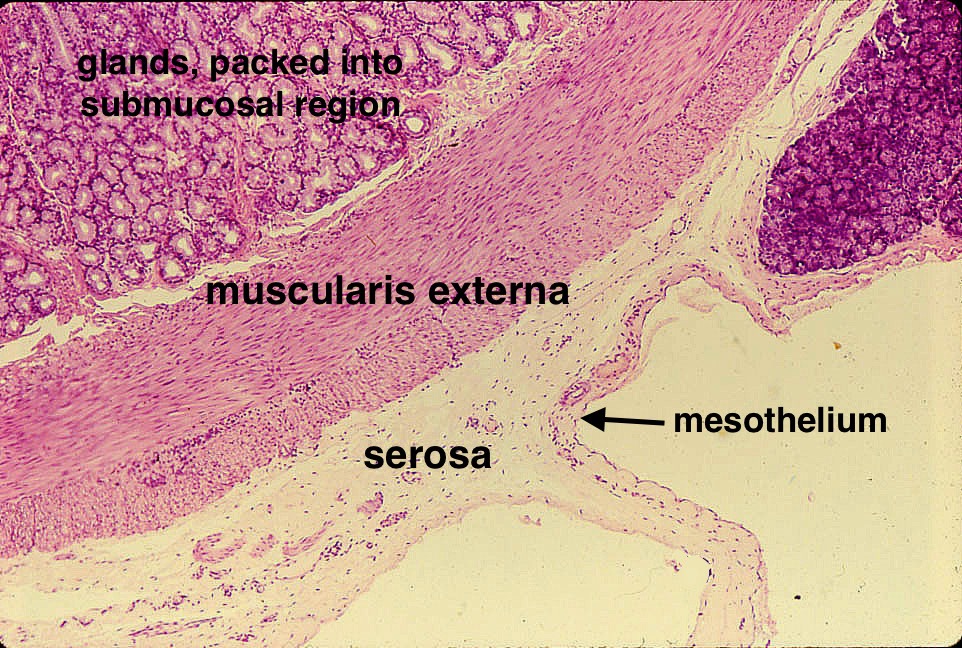
Some incidental vocabulary: The connective tissue that lies closest to an organ which it surrounds is commonly called adventitia. If the organ faces a body cavity (such as the intestine within the peritoneal cavity), the enwrapping connective tissue is called serosa, with a surface of mesothelium. If the surrounding connective tissue forms a tough enveloping sheet, it called an organ sheath. Connective tissue within a gland is called stroma. Much of remaining "everywhere" connective tissue is commonly called fascia, or just "ordinary connective tissue."
Many organs are built according to one of just two basic patterns of tissue architecture, the "tubular organ plan" and the "glandular organ plan" (These two plans might also be nicknamed "layers and lumps.")
- Examples of fundamentally tubular organs include those forming the entire gastrointestinal
tract, the upper respiratory tract, the urinary tract, the female and male reproductive tracts, and vessels of the circulatory system.
- Examples of organs built according to the glandular pattern are not just the obvious glands
such as salivary glands and pancreas but also lungs and kidneys and liver (although the liver displays
some curious departures from the basic glandular plan).
- A few organs (e.g., heart, spleen, brain) do not correspond with either of these two common histological plans.
Each organ has its own special details. Nevertheless, learning these two basic patterns -- the "tubular organ plan" and the "glandular organ plan" -- will cover a lot of territory all at one go, without the necessity of learning a special plan for each organ separately.
In both patterns, epithelium is supported by, or rests upon, connective tissue. In the tubular organ plan, epithelium forms the innermost lining of the tube. In the glandular plan, a vast area of epithelial surface (the parenchyma) is packed into a compact volume.
Tubular organs
 |
Layers of esophageal wall |
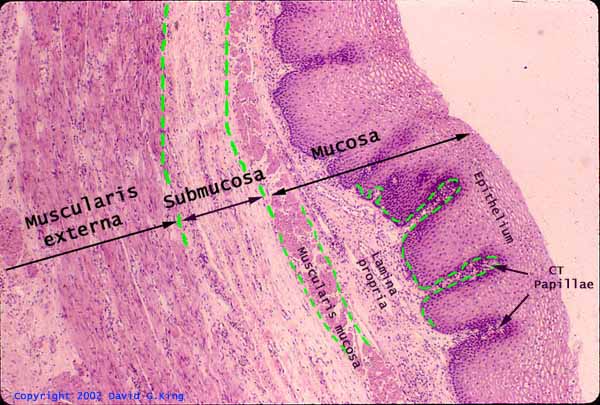
The basic tubular organ plan consists of three principal layers: the mucosa, the submucosa, and the muscularis externa. In effect, these layers form tubes within tubes. A fourth layer is also sometimes included in this list: the adventitia or the serosa.
- Mucosa is the layer adjacent to the lumen of a tubular organ. The mucosa includes the epithelial lining of the organ, with the specific type of epithelium being appropriate to the organ (e.g., stratified squamous epithelium for esophagus, simple columnar epithelium for intestine). The mucosa also includes a layer of connective tissue immediately beneath that epithelial lining, called lamina propria. The shape of the mucosal surface can be fairly elaborate, with wrinkles, pleats and villi; in some organs (e.g. stomach) the mucosa include many small mucosal glands.
- Submucosa comes next as we move deeper, farther away from the lumen. The name submucosa tells you
literally where it is: The submucosa lies beneath the mucosa. Submucosa is essentially just loose ordinary
connective tissue. The looseness of the submucosal connective tissue permits the deeper muscularis layer to
power peristalsis without tearing or putting strain on the relatively delicate mucosal lining. Blood vessels
in the submucosa are larger than those in the lamina propria. Both lamina propria and submucosa
are loose connective tissue; thus the boundary between mucosa and submucosa is somewhat arbitrary.
(Along most of the gastrointestinal tract, there is a thin layer of smooth muscle cells, called the muscularis
mucosae, at the boundary position.)
- Muscularis lies deeper still, beneath the submucosa. This layer is sometimes called the muscularis
externa, because it lies external to the inner layers of mucosa and submucosa. This smooth muscle layer is
responsible for peristalsis. Smooth muscle cells align with one another in bundles which share a common
orientation. In the muscularis, bundles typically orient with some fiber bundles encircling the tubular organ
while others run approximately parallel to the axis of the tube. In most regions of the gastrointestinal tract
the "circular muscle" and the "longitudinal muscle" form two distinct layers. In other tubular organs the orientation
of smooth muscle bundles is seldom so clear.
- Deeper connective tissue, loosely binding a tubular organ to surrounding fascia, is called adventitia. If the organ is adjacent to, or suspended within, a body cavity (e.g., like the intestine over much of its length) the connective tissue deep to the muscularis externa has a surface of mesothelium and is called serosa (image above).
Lamina propria -- the connective tissue layer of the mucosa -- is distinguished not only by position (immediately beneath the mucosal epithelium) but also by its connective tissue texture. Lamina propria generally has fewer, thinner collagen fibers and more numerous lymphocytes than deeper layers. Just how many lymphocytes is variable, but they tend to be noticeably more numerous where the overlying epithelium is more vulnerable and more involved in moving material across the epithelial boundary, such as the relatively delicate single layer of columnar cells that lines the intestine. Conversely, lymphocytes are much less numerous where the overlying tissue is a more protective stratified epithelium. Tiny foci of inflammation (recognized as small patches where lymphocytes are clustered) are relatively common in lamina propria.
 |
Layers of intestinal wall |
Layers of the tubular organ plan are clearly visible along most of the length of the gastrointestinal tract. These layers present their simplest appearance in the esophagus. For a more detailed description of the tubular organ plan, with additional images, see Tissue Layers of the GI Tract.
Glandular organs
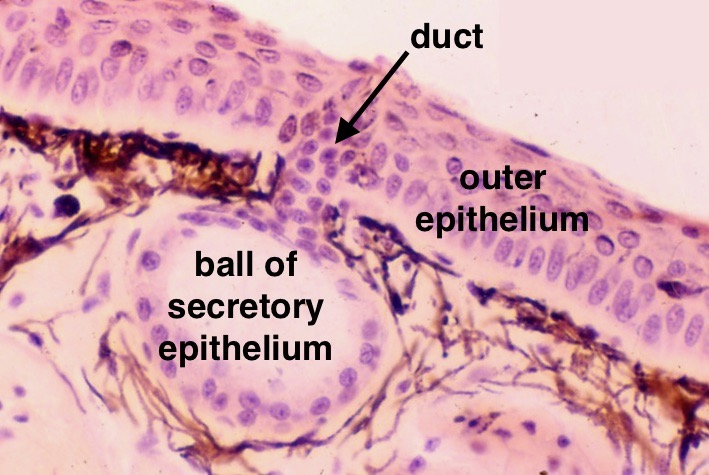
Glandular tissue architecture is nature's way of packing a relatively large epithelial surface area into a relatively small volume. Glandular architecture gives secretory cells access to the outside world by way of ducts, without actually exposing those cells to external hazards. A few organs not usually thought of as glands, notably the lung and the kidney, also share similar tissue organization (see below).
The epithelium of a gland follows the basic rules of epithelial tissue. Glandular epithelium forms a surface separating the space "above" the epithelium from connective tissue "beneath" the epithelium. The glandular epithelium is supported upon and sustained by that underlying connective tissue.
 |
Frog skin |

The basis for glandular architecture is exemplified by the extremely simple gland illustrated at left. At an orifice along an epithelial surface, that surface turns inward, forming a pore lined by duct epithelium. At its inner end, the duct is closed by a small ball of epithelial cells, called an acinus. The acinar cells are secretory, releasing their secretion into a lumen at the center of the acinus. The acinar lumen leads into the lumen of the duct. At the other end of the duct, at the pore, the duct lumen opens to the outside world. In the cartoon diagram at right, duct cells are colored blue and secretory epithelial cells are colored orange.

 Nature's trick for making a gland of substantial size, one which gives the appearance of a solid organ, is for a
relatively large duct to branch again and again into many small twigs. The end of each twig is capped by its own small
ball of secretory cells. (Think of grapes in a bunch.) Thus the ends of many, many little twigs of duct are capped
by many, many little acini. By branching repeatedly, a duct system can accommodate an extremely large number
of parenchymal cells. The result can be rather similar in shape to an
extremely large bunch of very tiny grapes (if the branching grape-stems were hollow ducts).
Nature's trick for making a gland of substantial size, one which gives the appearance of a solid organ, is for a
relatively large duct to branch again and again into many small twigs. The end of each twig is capped by its own small
ball of secretory cells. (Think of grapes in a bunch.) Thus the ends of many, many little twigs of duct are capped
by many, many little acini. By branching repeatedly, a duct system can accommodate an extremely large number
of parenchymal cells. The result can be rather similar in shape to an
extremely large bunch of very tiny grapes (if the branching grape-stems were hollow ducts).
Only secretory cells (orange) and duct cells (blue) are shown in the cartoons above. In those cartoons, stroma (connective tissue with blood vessels) occupies the area of background color. In a real gland (below), the acini are typically packed much more closely together (like the grapes in the bunch), such that supporting stroma is often inconspicuous (like the spaces between grapes in a bunch). In most actual glands, stroma occupies only a very small proportion of the overall bulk of the gland. Most of the gland's bulk is parenchyma (i.e., the secretory epithelial cells).
 |
Parenchyma of parotid gland |

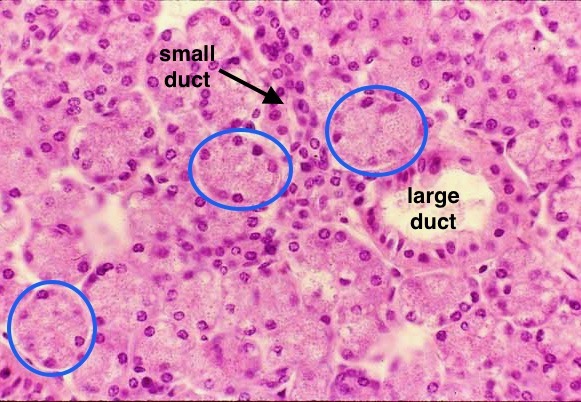
In the image of glandular parenchyma at left, many balls of secretory cells (acini) fill most of the field of view. Circled in blue are a few acini which happen to be fairly neatly cut in this section. Surrounding each acinus is the stroma, inconspicuous in these images, containing capillaries which provide material support for secretion. One acinus is enlarged at right. In this enlargment, the sides of individual parenchymal cells (where these cells attach to one another to form a continuous epithelial surface) are marked with white, and the central lumen of the acinus is indicated by an arrow. The central lumen of each acinus lies "outside" the epithelium. It communicates with the outside world through the gland's ducts.
For a more extensive description of the glandular organ plan, with additional images, see Histology of Glands.
Lung and kidney also share this basic architectural plan. In the lung, gas-exchange alveoli occupy the place of acini, with most of embryonic pulmonary epithelium transformed from cuboidal into extremely thin squamous cells. In the kidney, it is the duct tree's cuboidal epithelium that is elaborated into proximal and distal tubules of the renal parenchyma, with peculiar renal corpuscles in the position of glandular acini. In both of these organs, glandular-style stroma provides vascular support.
Other organs
A few organs (e.g., heart, spleen, brain) do not correspond with either of these two common histological plans.
For a much longer and more formal introduction to histology, see this page.
Histology Topics for Lincoln Scholars Program
