
 Histology Study Guide
Histology Study Guide
Respiratory Tract
These notes are an ancillary resource, NOT a substitute for scheduled
resource sessions or for textbooks. If you use this on-line
study aid, please refer to your textbooks and
atlases for richer, more detailed information.
SAQ
-- Self Assessment Questions
Preparation
Before studying the histology of any particular system or organ, one should
appreciate the basic concepts and tools of histology, as presented in the
Introduction to Histology at this
website. In particular, one should be familiar with the four
basic tissue types, most especially epithelium
and connective tissue and with the basic tools
of histology.
Overview of Respiratory Tract Histology
The lung is one of several organs that packs a large epithelial surface
area into a compact volume. The basic organizational pattern is that
of a gland, in which a branching tree of
tubes provides continuity from the body's outside surface to a vast number
of epithelial cells.
- Indeed, the respiratory tract begins life as an invagination of
epithelial (endodermal) tissue. Embryonic lungs even have
the histological appearance of glands (see
Webpath).
Only fairly late in development do the cuboidal epithelial
cells of the terminal alveoli assume the thin
squamous epithelial shape that characterizes
the lining of mature gas-exchanging air sacs. (Some significant secretory
function is retained, in the form of cuboidal, surfactant-producing great
alveolar cells.)
- In the respiratory system, just as in large glands, a
system of conducting passageways form a branching "tree," with
functional units at the end of each twig.
- In the respiratory system, the tree's "trunk"
is the trachea, larger branches are called bronchi
(singular "bronchus"), and smaller branches are called
bronchioles. (In a gland,
the conducting passages are called "ducts.")
- In the lung, the epithelial cells
at the ends of all the twigs form "respiratory units," also
called alveoli (singular, "alveolus").
In a gland, the secretory units
at the ends of the twigs are also sometimes called "alveoli,"
which means a small hollow or cavity.
The pleural cavity is lined by mesothelium. This includes both
the outer surface* of lung and the adjacent inner surface* of the chest wall.
(Simple squamous mesothelial tissue also lines the other major body cavities,
pericardial and peritoneal.)
* Note that "outer surface" in the above paragraph refers to the surface that a surgeon encounters upon opening
the ribcage, while "inner surface" refers to the gas-exchange membranes "inside" the lung. These "inner" surfaces
actually face inspired air, and are therefore more properly the "outer" surfaces of alveolar epithelium.

 The conducting passageways of the respiratory system (nasal cavity, trachea,
bronchi and bronchioles)
are lined by pseudostratified columnar
epithelial tissue, which is ciliated and which includes mucus-secreting
goblet cells. Incoming particulates (dust, bacteria) adhere to
the mucus, which is then swept upward and away by the cilia.
The conducting passageways of the respiratory system (nasal cavity, trachea,
bronchi and bronchioles)
are lined by pseudostratified columnar
epithelial tissue, which is ciliated and which includes mucus-secreting
goblet cells. Incoming particulates (dust, bacteria) adhere to
the mucus, which is then swept upward and away by the cilia.
An extensive vascular plexus allows heat-exchange to condition air before
it reaches the delicate alveoli.
Because the passage of air depends on wide open passageways, the larger respiratory
passages (trachea, and bronchi)
are held open by supportive skeletal elements made of cartilage.
 The respiratory, gas-exchange surface consists of simple squamous
epithelium lining millions of small sacs, called alveoli. Between adjacent alveoli
is a network of capillaries. The epithelium lining each alveolus is exceedingly thin to facilitate diffusion
of oxygen and CO2 across that lining into blood. This gas-exchange function of this pulmonary
vasculature is critical to organ function and to life itself. (Alveolar epithelium also contain cuboidal
surfactant-secreting cells. The surfactant overcomes the tendency of
alveolar walls to adhere to one another, which would obliterate the air space).
The respiratory, gas-exchange surface consists of simple squamous
epithelium lining millions of small sacs, called alveoli. Between adjacent alveoli
is a network of capillaries. The epithelium lining each alveolus is exceedingly thin to facilitate diffusion
of oxygen and CO2 across that lining into blood. This gas-exchange function of this pulmonary
vasculature is critical to organ function and to life itself. (Alveolar epithelium also contain cuboidal
surfactant-secreting cells. The surfactant overcomes the tendency of
alveolar walls to adhere to one another, which would obliterate the air space).
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
Nasopharynx
The nasal cavity, like the rest of the larger respiratory passageways,
is lined by ciliated, pseudostratified
columnar epithelium with goblet cells.
The olfactory mucosa is lubricated by Bowman's glands (named after William Bowman, b. 1816).
The mucosal surfaces of the nasal passages are important for conditioning
air before it reaches the more-delicate alveolar tissue. Many small
glands provide moisture-containing mucus for humidification as well as for capturing incoming
dust. A vascular plexus facilitates heat exchange.
The most distal expression of this heat-exchange mechanism is found in Little's area
(commemorating James Little, b. 1836),
located inside the nose just beneath the anteroinferior epithelial surface of the nasal septum. Also known as
Kiesselbach's area (commemorating Wilhelm Kiesselbach,
b. 1839), this site contains arterial anastomoses (Kiesselbach's plexus). Delicacy
of the overlying epithelium makes this relatively-exposed site a frequent source of nosebleeds.
Have you ever noticed what a big nose a camel has?
Nasal air-conditioning is especially effective in this animal.
When the creature inhales, hot dry desert air is humidified by evaporation
of nasal secretions, while the nasal passages themselves are chilled by
evaporative cooling. During exhalation, the cooled passages condense
and recover some of the moisture, thereby contributing to water conservation.
In our own bodies, air conditioning is not as effective
as that of the camel. But evaporative cooling of the respiratory passages
does provide a significant contribution to thermoregulation during vigorous
exercise. (In other words, many of the calories expended during exercise
do not do any useful work but only generate heat, which in turn evaporates water into the air that we exhale.)
Pseudostratified respiratory epithelium begins in the nasal cavity
and continues with minor variations through the nasopharynx and down
the trachea, bronchi and bronchioles.
 The contrast between respiratory epithelium of the nasopharynx and the
stratified squamous epithelium of the oral cavity can be seen in a cross-section
of the palate (or, similarly, a cross section of the epiglottis).
The contrast between respiratory epithelium of the nasopharynx and the
stratified squamous epithelium of the oral cavity can be seen in a cross-section
of the palate (or, similarly, a cross section of the epiglottis).
 One small region of the nasal cavity, the olfactory mucosa, has a highly
modified epithelium containing specialized sensory receptor cells. Although
the olfactory receptors have the superficial appearance of columnar epithelial cells (and indeed are regularly
replaced by newly divided cells, as is typical for cells forming many other epithelia surfaces),
these olfactory receptor s are essentially nerve cells. Each olfactory receptor cell carries
at its apical end a peculiar knob or "olfactory vesicle" from which
sprout several long but non-motile cilia. (For EM images of this remarkable structure,
see the Electron Microscopic
Atlas.)
Each olfactory cell also has an axon which extends from the basal end of the
cell to the olfactory bulb of the brain. The many axons from olfactory
receptors pass through the medial portion of the ethmoid bone that is called
the cribriform plate ("cribriform" means "like a sieve,"
i.e., full of holes).
One small region of the nasal cavity, the olfactory mucosa, has a highly
modified epithelium containing specialized sensory receptor cells. Although
the olfactory receptors have the superficial appearance of columnar epithelial cells (and indeed are regularly
replaced by newly divided cells, as is typical for cells forming many other epithelia surfaces),
these olfactory receptor s are essentially nerve cells. Each olfactory receptor cell carries
at its apical end a peculiar knob or "olfactory vesicle" from which
sprout several long but non-motile cilia. (For EM images of this remarkable structure,
see the Electron Microscopic
Atlas.)
Each olfactory cell also has an axon which extends from the basal end of the
cell to the olfactory bulb of the brain. The many axons from olfactory
receptors pass through the medial portion of the ethmoid bone that is called
the cribriform plate ("cribriform" means "like a sieve,"
i.e., full of holes).
Olfactory epithelial cells are quite wonderful, even beyond their utterly
bizarre shape that displays elements of both epithelial and neural form.
Renowned physician-essayist Lewis
Thomas chose these cells as one of the "Seven Wonders of the Modern
World":
"My Fifth Wonder is the olfactory receptor cell,
located in the epithelial tissue high in the nose, sniffing the air for
clues to the environment, the fragrance of friends, the smell of leaf
smoke, breakfast, nighttime and bedtime, and a rose, even, it is said,
the odor of sanctity. The cell that does all these things, firing
off urgent messages into the deepest parts of the brain, switching on
one strange unaccountable memory after another, is itself a proper brain
cell, a certified neuron belonging to the brain but miles away out in
the open air, nosing around the world. How it manages to make sense of
what it senses, discriminating between jasmine and anything else non-jasmine
with infallibility, is one of the deep secrets of neurobiology.
This would be wonder enough, but there is more. This population
of brain cells, unlike any other neurons of the vertebrate central nervous
system, turns itself over every few weeks; cells wear out, die, and are
replaced by brand-new cells rewired to the same deep centers miles back
in the brain, sensing and remembering the same wonderful smells.
If and when we reach an understanding of these cells and their functions,
including the moods and whims under their governance, we will know a lot
more about the mind than we do now, a world away." [Lewis Thomas,
Seven Wonders, pp. 55-63, in Late Night Thoughts on Listening
to Mahler's Ninth SymphonyViking Press, 1983.]
Consult your histology textbook and/or atlas (e.g., Rhodin, figures
31-5 to 31-8) for additional detail and electron micrographs
of olfactory cells.
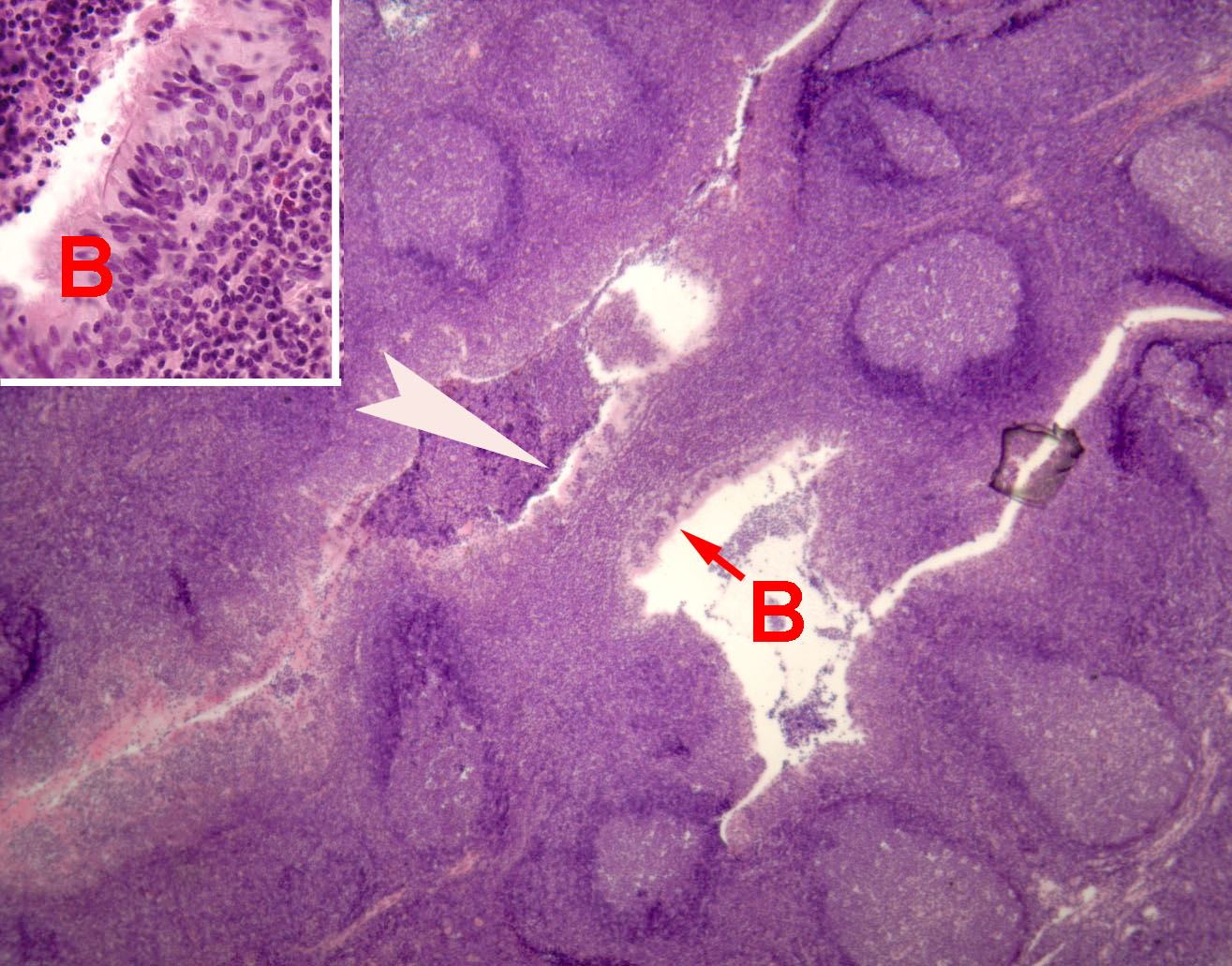
The pharynx houses tonsils, which are localized lymphoid specializations
located in the mucosa not only of the pharynx
but also of the tongue and the palate. Each tonsil consists of an epithelial
crypt (an invaginated pocket) surrounded by dense clusters of lymph
nodules.
Lymph nodules (also called lymphoid follicles) are sites
where lymphocytes congregate.
At the center of each lymph nodule is a "germinal center" where the lymphocytes
proliferate.
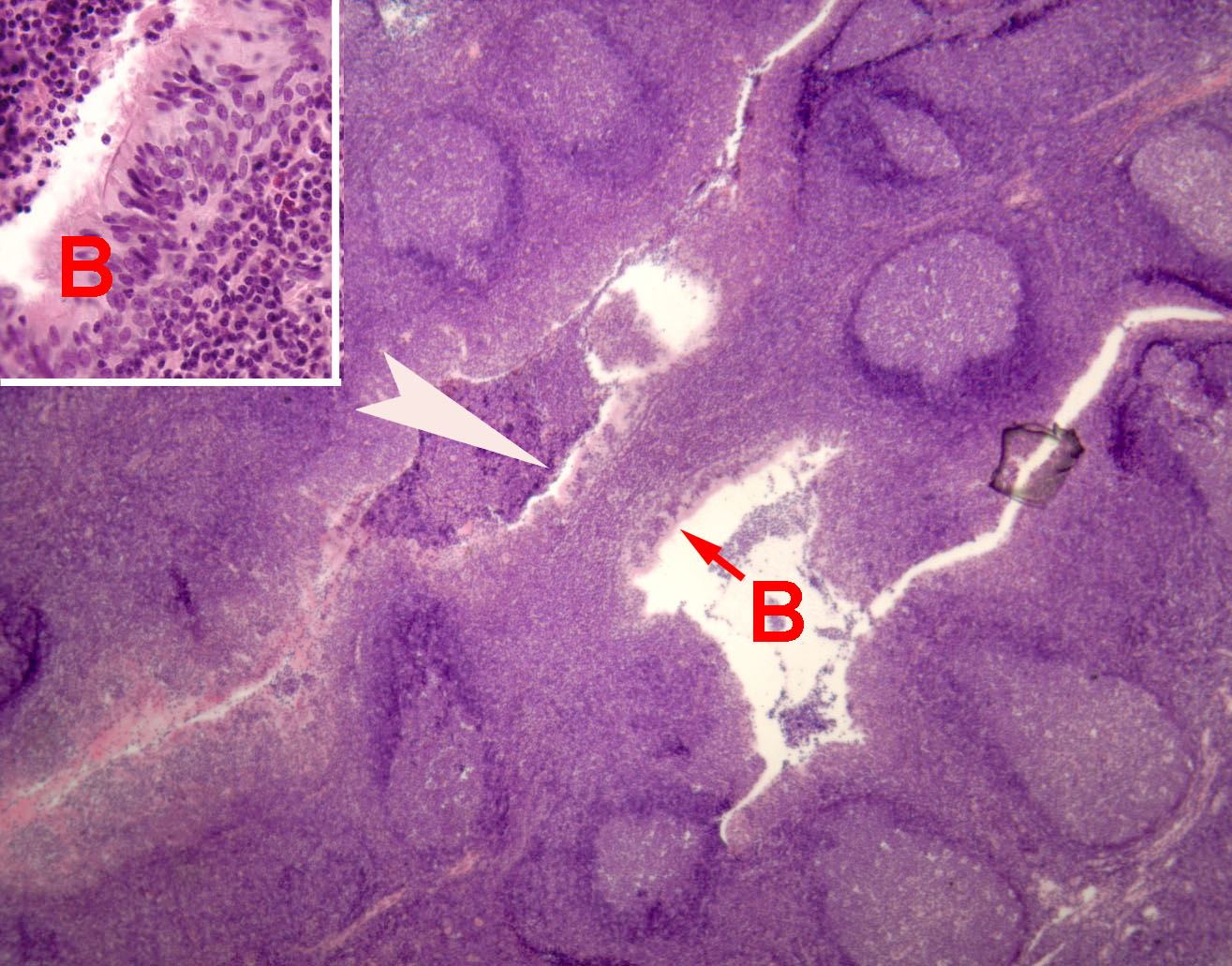 Pharyngeal tonsils (also called "adenoids") provide
immune surveillance cells (lymphocytes)
with sites for encountering foreign antigens which enter the body through inspired
air.
Pharyngeal tonsils (also called "adenoids") provide
immune surveillance cells (lymphocytes)
with sites for encountering foreign antigens which enter the body through inspired
air.
For more on Mucosa-Associated Lymphoid Tissues (MALT),
consult your histology and immunology texts.
 Pharyngeal tonsils resemble those of the palate (palatine
tonsils, thumbnail to right), but with ciliated, pseudostratified columnar
epithelium rather than stratified
squamous epithelium lining the surface and crypts.
Pharyngeal tonsils resemble those of the palate (palatine
tonsils, thumbnail to right), but with ciliated, pseudostratified columnar
epithelium rather than stratified
squamous epithelium lining the surface and crypts.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
Conducting
system.
Most of the larger respiratory passageways, from the nasal cavity through the bronchi,
are lined by a pseudostratified
columnar epithelium.
 This respiratory epithelium consists primarily of columnar ciliated cells interspersed with mucus-secreting
goblet cells. Ciliary beating sweeps mucus and the dust it carries up the bronchi
and trachea toward the pharynx, where it can be swallowed.
This respiratory epithelium consists primarily of columnar ciliated cells interspersed with mucus-secreting
goblet cells. Ciliary beating sweeps mucus and the dust it carries up the bronchi
and trachea toward the pharynx, where it can be swallowed.
Further down the tree, the columnar epithelium of trachea and bronchi transitions to simple cuboidal
epithelium of bronchioles. The height of this epithelium decreases as one descends bronchiolar
branches toward gas-exchange regions. (Lung alveoli, in
contrast, are lined by very thin simple
squamous epithelium.)
Electron micrographs of cilia may be seen at WebPath
and at the Electron Microscopic Atlas.
(A ciliated epithelium is also characteristic the
female reproductive tract.)
 Scattered among the ciliated cells are occasional mucus-secreting goblet cells.
Mucus moistens the epithelial surface (so the ciliated cells
can function) and adheres to inhaled particles (so dust and bacteria are caught
before they are carried all the way into alveoli).
Scattered among the ciliated cells are occasional mucus-secreting goblet cells.
Mucus moistens the epithelial surface (so the ciliated cells
can function) and adheres to inhaled particles (so dust and bacteria are caught
before they are carried all the way into alveoli).
For additional detail on the properties of respiratory mucous
in relation to ciliary function, see B. F. Dickey (2012) Walking on Solid
Ground, Science,
24 August 2012: 924-925..
The name "goblet cell" refers to the cell's shape:
narrow at the base and bulging apically. The apical end of each goblet
cell is occupied by a large mass of mucus, which compresses adjacent
cells (thus conferring the characteristic "goblet" shape) and
displaces the nucleus toward the basal end of the cell. As in other
mucous cells, the nucleus is compact
and intensely stained (basophilic) with H&E.
(Mucus-secreting cells of similar shape, also called "goblet cells," may be found
in the gastrointestinal
tract.)
Basal cells (those whose nuclei lie low in the epithelium, near the
basement membrane) are believed to be the source of replacement ciliated and
goblet cells.
 In our slide set, ciliated respiratory epithelium is best represented by slides
of the trachea (or "trachea and esophagus").
In our slide set, ciliated respiratory epithelium is best represented by slides
of the trachea (or "trachea and esophagus").
Consult your histology textbook and/or atlas (e.g., Rhodin,
figure 31-22) for additional detail and electron micrographs
of these cells.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
Trachea, bronchi, and
bronchioles
|
|
The trachea is the "trunk" of the branching tree of
passageways leading into the lungs. Its major histological specializations
include skeletal reinforcement in the form of incomplete (i.e., C-shaped)
rings of cartilage and a
vascular (venous) plexus which facilitates heat exchange to condition
air before it reaches the delicate alveoli.
For details of the ciliated, pseudostratified epithelium
of the trachea, see above.
|
 |
|
The trachea divides into two primary bronchi (singular,
bronchus), one to each lung. The
primary bronchi then divide repeatedly into smaller bronchi and even smaller
bronchioles. Thus bronchi and bronchioles are,
respectively, the larger and smaller branches of the
air-conducting tree extending into the lung.
|
 |
 |
Several parameters -- the amount of cartilage, the thickness of the respiratory
epithelium, and the degree of pseudostratification -- all decrease as one
descends the air-conducting passages toward the alveoli.
|
|
The distinction between bronchi and bronchioles is somewhat arbitrary,
but in general bronchi
have cartilagenous reinforcement and a columnar epithelial lining, while
bronchioles lack cartilage and have a simple
cuboidal lining.
Besides ciliated and mucus-secreting cells (see above), bronchiolar epithelium may
include club cells (bronchiolar exocrine cells) whose role remains incompletely understood but which seem to
have some specialized synthetic and secretory function.
Research review: Rokicki, Wojciech et al. (2016), "The role
and importance of club cells (Clara cells) in the pathogenesis
of some respiratory diseases," Kardiochirurgia i torakochirurgia polska = Polish journal of cardio-thoracic surgery,
vol. 13, pp. 26-30. doi:10.5114/kitp.2016.58961.
Historical note: Older textbooks refer to bronchiolar exocrine
cells as "Clara cells," a name which recognizes
researcher Max Clara (b. 1899) who worked on bodies of prisoners executed by the Nazi regime prior
to WWII (e.g. see here).
Because of this tainted history, the alternative term "club cells"
has been adopted by several journals and societies.
|
 |
 |
Consult your histology textbook and/or atlas
(e.g., Rhodin, figures 31-35 to 31-40) for additional
detail and electron micrographs of bronchial
and bronchiolar cells.
|
|
Small mucous glands are scattered along most of the respiratory
tree and may occasionally be seen in the wall of bronchi or bronchioles.
The airway walls also
feature smooth muscle, which permits
regulation of the distribution of air through the lung's volume.
|
 |
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
 Respiratory (gas-exchange) region of lung
Respiratory (gas-exchange) region of lung
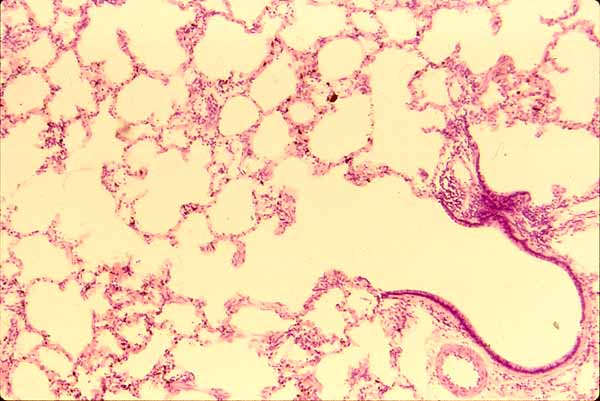
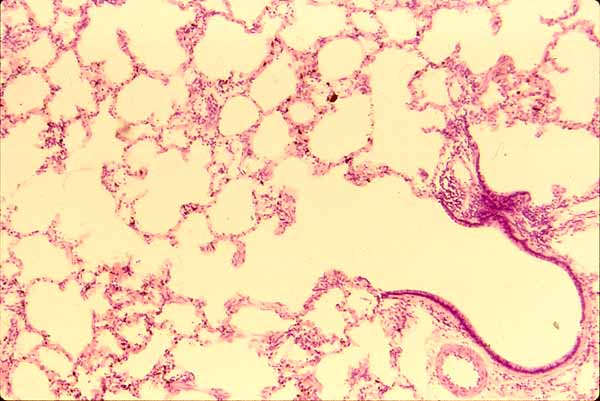
The lung consists of functional respiratory units called "air sacs"
or alveoli (singular, alveolus),
 each connected via bronchioles and bronchi
to the trachea.
each connected via bronchioles and bronchi
to the trachea.
Because the actual shape of the gas-exchange spaces is somewhat complex,
additional descriptive terminology is sometimes used. Terminal bronchioles,
those which open directly into gas-exchange spaces, are called respiratory
bronchioles. These typically open into passageways, called respiratory
ducts, that open not only into alveoli but also into further passageways,
called respiratory sacs, that themselves open into more alveoli.
In elementary science classes, the
lung is sometimes misleadingly portrayed as a balloon at the end of a large
bronchus. There is no balloon. One
might imagine that each alveolus is a very tiny balloon, but even this is
not accurate. The lung is more like a well-organized sponge. Each alveolus
shares its wall (inter-alveolar septum) with adjacent alveoli. Alveoli
cannot collapse individually, only all together.
Note on clinical histology:
The lung's normal volume is mostly air-filled space. In ideal
histological specimens, this space is preserved by keeping the lung inflated
during preparation. But as a matter of convenience, clinical specimens
are often prepared in a somewhat collapsed state. Do not be surprised
by lung specimens in which alveoli appear flattened, with alveolar walls
wrinkled and pressed together, with reduction in the air-space.


Alveoli
are separated from one another by thin alveolar walls (interalveolar septa).
Each alveolus is lined by simple
squamous epithelium, exceedingly thin to facilitate diffusion of oxygen
while still forming an epithelial barrier between the outside air and the
internal body fluids.
In between the epithelial surfaces of adjacent alveoli lies a network of capillaries,
through which flow the red blood cells whose hemoglobin absorbs oxygen for
transport to the rest of the body (also see lung vasculature, below).
In other words, each interalveolar septum consists of simple
squamous epithelium on either side with capillaries
sandwiched in between.
 Before being absorbed by hemoglobin, an oxygen molecule
must first reach an alveolus, then diffuse across the plasma membrane of
a squamous epithelial cell, through the very thin epithelial cell cytoplasm,
across the plasma membrane on the other side of the epithelial cell, across
the basement membrane which separates the epithelium from the underlying
tissue, across the basement membrane which surrounds each capillary
(these two basement membranes may be fused together), across the plasma
membrane of a capillary endothelial cell,
through the very thin cytoplasm of this cell, across the plasma membrane
on the capillary-lumen side of the endothelial
cell, through a bit of blood plasma, and finally across the membrane
of a red blood cell. Whew! The total thickness may be less than 0.05 μm.
Before being absorbed by hemoglobin, an oxygen molecule
must first reach an alveolus, then diffuse across the plasma membrane of
a squamous epithelial cell, through the very thin epithelial cell cytoplasm,
across the plasma membrane on the other side of the epithelial cell, across
the basement membrane which separates the epithelium from the underlying
tissue, across the basement membrane which surrounds each capillary
(these two basement membranes may be fused together), across the plasma
membrane of a capillary endothelial cell,
through the very thin cytoplasm of this cell, across the plasma membrane
on the capillary-lumen side of the endothelial
cell, through a bit of blood plasma, and finally across the membrane
of a red blood cell. Whew! The total thickness may be less than 0.05 μm.
An electron micrograph of the blood-air barrier
may be seen at the Electron Microscopic Atlas.
Clinical note: Alveoli can provide a cozy
haven for bacterial growth, leading to pneumonia and inflammation.
For an image of alveoli filled with inflammatory cells, see WebPath.
(For additional lung pathology, see below.)
The squamous epithelial cells of the alveolar walls are sometimes called Type
I pneumocytes. As noted above, these squamous
Type I cells facilitate gas exchange.
Scattered among the squamous cells are occasional larger cuboidal cells,
sometimes called greater alveolar cells and sometimes called Type
II pneumocytes. These cells secrete surfactant, which serves the
critical function of keeping alveolar walls from sticking to one another.
Consult your histology textbook and/or atlas (e.g., Rhodin,
figures 31-45 to 31-54) for additional detail and electron
micrographs of cells associated with lung alveoli.
See the Electron Microscopic Atlas for (mostly unlabelled) EM images of lung.
 The edges of inter-alveolar septa, at the entry-ways into respiratory sacs and alveoli,
contain small bundles of smooth muscle which
allow some control of air distribution among various regions of the lung.
The edges of inter-alveolar septa, at the entry-ways into respiratory sacs and alveoli,
contain small bundles of smooth muscle which
allow some control of air distribution among various regions of the lung.
 To keep the alveoli clean, amoeboid phagocytic cells crawl over the surface of
the alveolar walls and ingest any foreign material that they encounter.
These cells are sometimes called "dust cells," but they are basically alveolar
macrophages that have moved out
of connective tissue and onto the epithelial surface of the alveoli.
To keep the alveoli clean, amoeboid phagocytic cells crawl over the surface of
the alveolar walls and ingest any foreign material that they encounter.
These cells are sometimes called "dust cells," but they are basically alveolar
macrophages that have moved out
of connective tissue and onto the epithelial surface of the alveoli.
It is perhaps amusing to note that
these cells are behaving rather like independent agents, having left the
body proper by crossing the alveolar epithelium. Although they may
again cross the epithelium and re-enter the body, these cells may also be
swept up the airway by cilia and swallowed, in effect becoming food.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
Lung vasculature

 Larger
vessels, both veins and arteries,
tend to follow the same branching tree as the airways, so the connective tissue
around each bronchus and bronchiole typically contains
an artery and a vein.
Larger
vessels, both veins and arteries,
tend to follow the same branching tree as the airways, so the connective tissue
around each bronchus and bronchiole typically contains
an artery and a vein.
Because pulmonary circulation has lower pressure
than systemic circulation, pulmonary arteries and veins tend to have more
delicate walls than those seen elsewhere in the body.


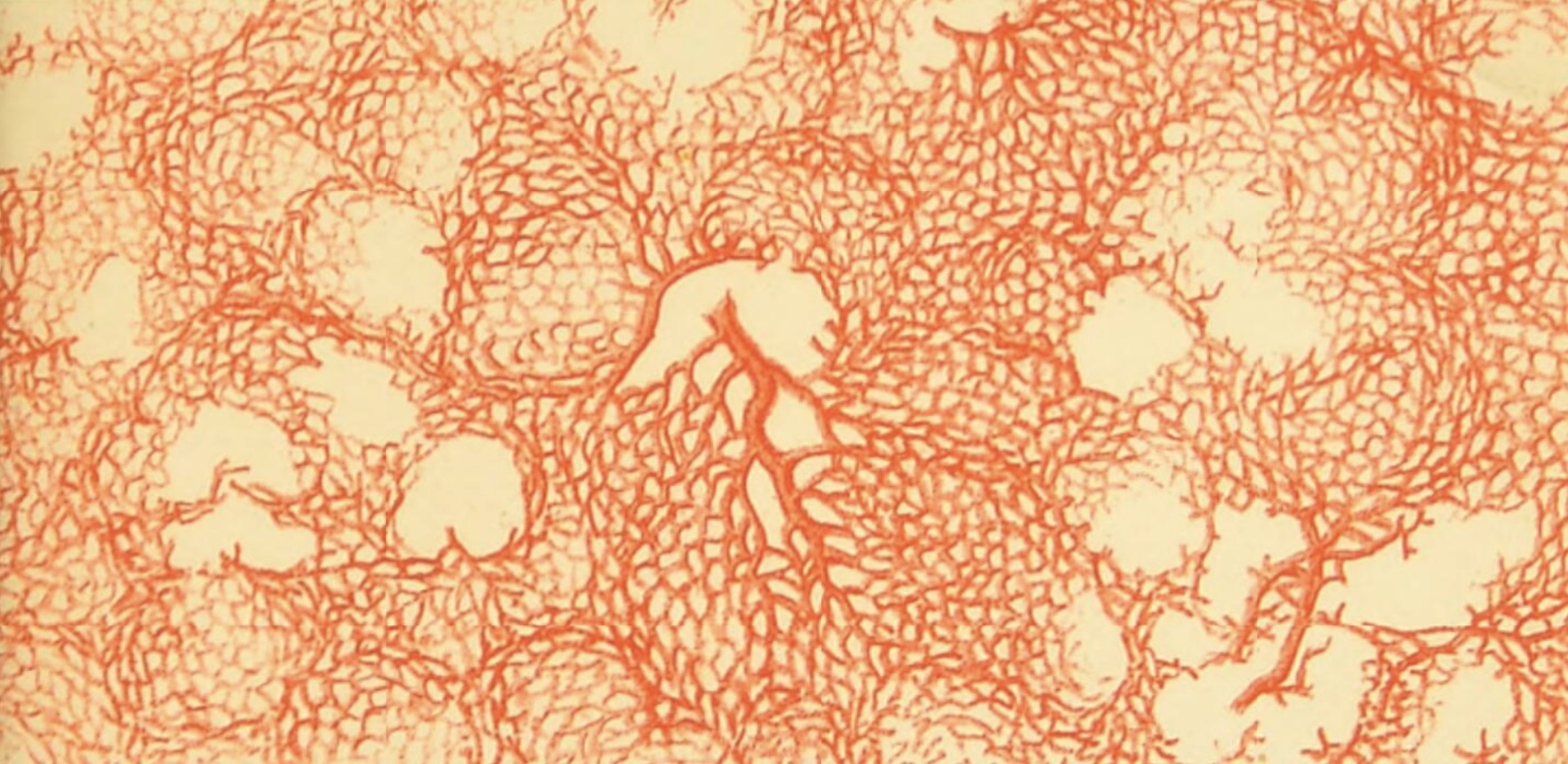
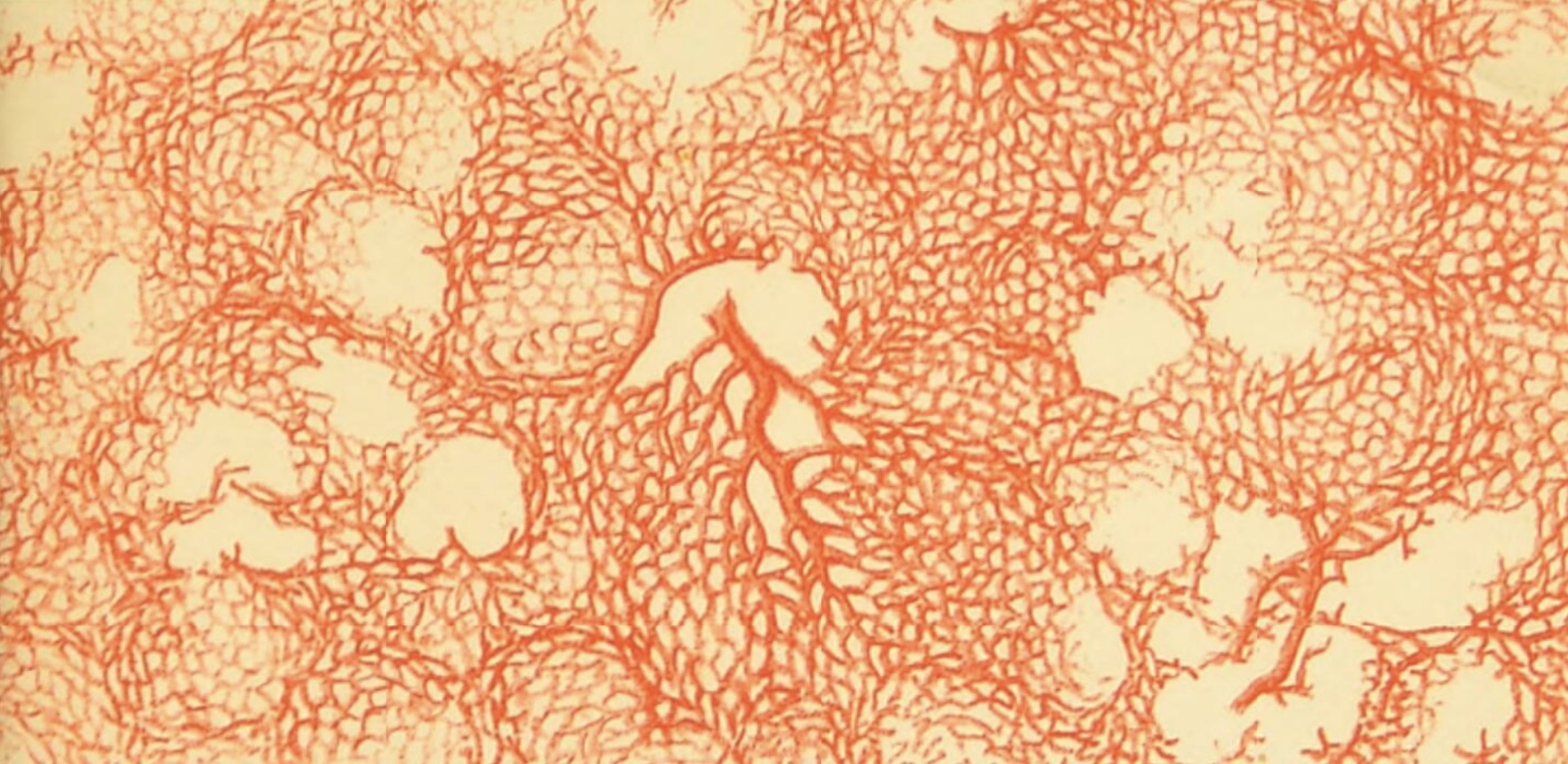
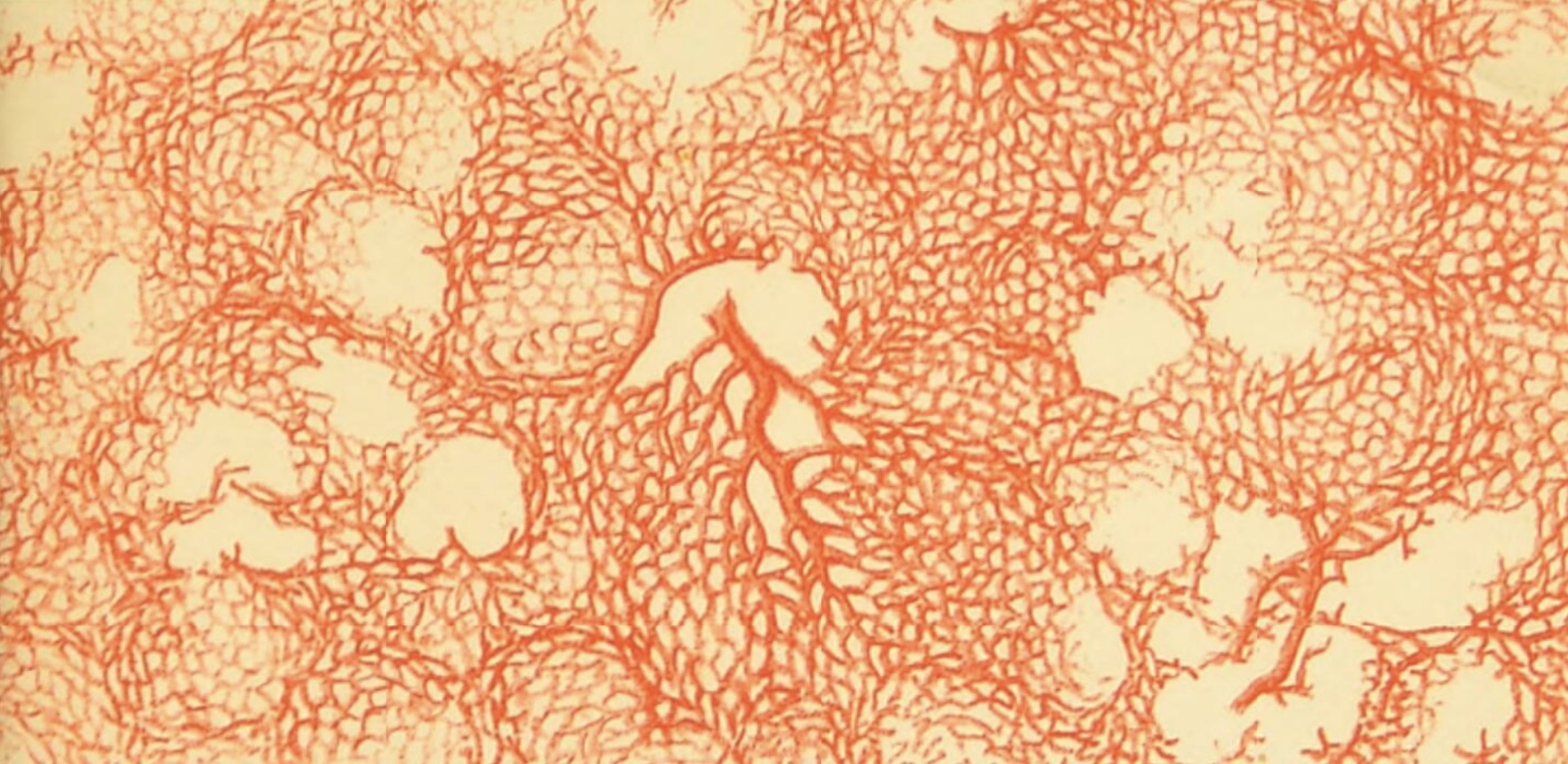 The essential gas-exchange function of lung can only be carried out because alveolar
walls are richly supplied with capillaries (see gas-exchange region,
above). Indeed, most of the "bulk" of the alveolar walls consists
of the blood cells which are passing through these capillaries. Alveolar capillaries are continuous (i.e.,
NOT fenestrated) so that fluid cannot normally leak out of blood and into air spaces.
The essential gas-exchange function of lung can only be carried out because alveolar
walls are richly supplied with capillaries (see gas-exchange region,
above). Indeed, most of the "bulk" of the alveolar walls consists
of the blood cells which are passing through these capillaries. Alveolar capillaries are continuous (i.e.,
NOT fenestrated) so that fluid cannot normally leak out of blood and into air spaces.
Historial note: William Harvey (b. 1578), who first
understood the circulation of blood, lacked the means to directly observe the capillary connections between artieries and
veins. Capillaries were first reported a few years after Harvey's death, by Marcello
Malpighi (b. 1628), based on his microscopic observations of frog lung.
Consult your histology textbook and/or atlas (e.g., Rhodin,
figures 31-55 to 31-67) for additional detail and electron
micrographs of pulmonary vessels.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / RESPIRATORY IMAGE INDEX
Examples of pulmonary pathology,
The following links illustrate some departures from normal lung-tissue appearance,
presented at the WebPath
website. In these images, try to recognize the basic features of lung
tissue as well as the particular pathology.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE
Image index
 Comments
and questions: dgking@siu.edu
Comments
and questions: dgking@siu.edu
SIUC / School
of Medicine / Anatomy / David
King
https://histology.siu.edu/crr/rsguide.htm
Last updated: 13 July 2023 / dgk
 Histology Study Guide
Histology Study Guide Introduction / overview
Introduction / overview Conducting system (air passageways)
Conducting system (air passageways)
 Respiratory
region
Respiratory
region















 Comments
and questions:
Comments
and questions: