
 Histology Study Guide
Histology Study Guide
Cardiovascular System
These notes are an ancillary resource, NOT a substitute for scheduled
resource sessions or for textbooks. If you use this on-line
study aid, please refer to your textbooks and
atlases for richer, more detailed information.
SAQ -- Self Assessment Questions
SAQ, Cardiovascular
and Lymphatic Systems
SAQ, Introduction -- microscopy, cells,
basic tissue types, blood cells.
Blood vessels
 Blood vessels are basically tubular organs found within other organs.
(Recall that an "organ" consists of two or more different tissue
types "organized" to serve a larger function.)
Blood vessels are basically tubular organs found within other organs.
(Recall that an "organ" consists of two or more different tissue
types "organized" to serve a larger function.)
Larger blood vessels may even have smaller vessels within
their walls (the vasa vasorum).
|
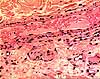
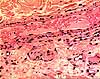
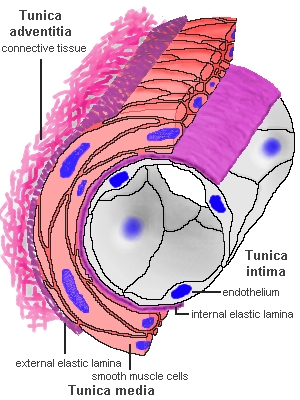 Histologically,
blood vessels consist of concentric layers or "tunics"
of different tissue types. Histologically,
blood vessels consist of concentric layers or "tunics"
of different tissue types.
- The tunica intima is the inner lining, consisting
of endothelium and a relatively thin layer
of supporting connective tissue.
- The tunica media is the middle muscular and/or
elastic layer, containing smooth muscle
and elastic tissue in varying proportions.
- The tunica adventitia is the outer, fibrous
connective tissue layer.
- Nervous tissue is generally inconspicuous in blood vessels but serves
to regulate smooth muscle function and to mediate pain sensation.
Image ©
Blue Histology
|
Blood vessels are categorized by function. Different categories of vessels differ somewhat in the detailed composition of their layers.
- Note that arteries and veins tend to travel together,
so histological sections often provide opportunities to compare an adjacent
vein/artery pair.
- Arteries conduct blood away from the heart
and have proportionately more smooth muscle and elastic tissue than veins
of comparable size.
- Arteries are commonly sub-categorized into elastic
arteries, muscular arteries, and arterioles.
- Veins return blood to the heart and have proportionately
less smooth muscle and elastic tissue than arteries of comparable size.
- Capillaries and sinusoids
communicate between arteries and veins. Their lining generally consists
only of endothelium and underlying basement
membrane.
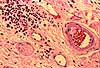
Note that capillaries are found in connective tissue
(or stroma) in nearly every organ (cartilage is an exception, an avascular
connective tissue), but capillaries are seldom noticable in routine histological
sections.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
 Intima
(tunica intima)
Intima
(tunica intima)
Historical note: The tunica intima is also called Bichat's
tunic," after Xavier Bichat (b. 1771), "the Father of Histology."
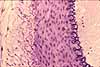
The intima is the inner layer of a vessel. It consists of very
thin lining of simple squamous endothelial cells supported by a similarly
thin layer of connective tissue. The integrity of the intima is critical,
since damage can lead to atherosclerosis or clotting.
- In arteries a continuous layer of elastic
tissue, called the internal elastic lamina, forms the boundary
between the intima and the media.
Endothelium

 The
endothelium is a specialized form of mesenchymally-derived epithelial
tissue. This simple squamous
epithelium forms a thin, delicate lining of all blood vessels as well
as the heart and the lymphatic system.
The endothelium is arguably the most significant feature of the vessel.
The
endothelium is a specialized form of mesenchymally-derived epithelial
tissue. This simple squamous
epithelium forms a thin, delicate lining of all blood vessels as well
as the heart and the lymphatic system.
The endothelium is arguably the most significant feature of the vessel.
Capillary endothelium may have closely associated pericytes,
cells with contractile properties which might regulate capillary flow.
Endothelial cytoplasm is inconspicuous in routine light microscopy. Typically
only the nuclei are noticeable, at the boundary between the lumen and the wall
of a vessel.
In cross section, endothelial nuclei
typically appear thin and dark. However, occasionally endothelium
lies parallel to the plane of section. In this case the nuclei may
appear very large, round, and pale.
Although endothelial cells appear rather uninteresting
under the microscope, these are important cells. They are situated
at a critical location, between the blood and all other body cells. They
secrete substances which control local blood flow and blood coagulation,
and they are active participants in white blood cell emigration during inflammation.
Historical note: The close association of
endothelium with macrophages in liver, spleen
and lymph nodes (i.e., those organs with elaborate
endothelially-lined channels supported by reticular
connective tissue) led to the term reticuloendothelial system.
The name reflects former confusion about the distinction between
endothelial cells and the scattered population of macrophages (monocytes,
histiocytes). Macrophages can be readily labelled through
their phagocytosis of experimentally-injected carbon particles. However, endothelial
cells are also labelled by the same procedure. Although endothelial
cells are not dramatically phagocytotic, they do shuttle some materials
across the endothelial lining via small endocytotic and exocytotic vesicles.
Continuous endothelium. Throughout much of the body, the capillary
endothelial lining is continuous, with neither large gaps between cells
nor holes through cells. Materials pass across the endothelium either
by diffusion or via rapid vesicular transcytosis. (In most of the brain,
a lack of transcytotic vesicles accounts for the blood brain barrier -- the
only substances which cross such a barrier are those which can diffuse through
plasma membranes or those for which specific membrane channels exist.)
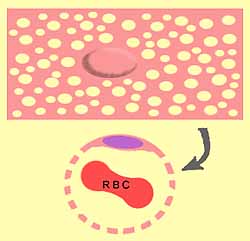
Fenestrated endothelium. In a few special locations -- notably
in the sinusoids of the liver, in
the glomeruli of the kidney, and
in most endocrine glands -- the endothelium
is fenestrated (i.e., full of holes -- from fenestra, window; see cartoon image at right).
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of endothelial cells.
- Variations in the endothelial lining determine how freely blood components
can leave the vessel (see capillaries).
- Perhaps even more critically (at least from a clinical perspective), the
endothelium must allow blood to flow freely past without any disturbance
that might trigger clotting. And yet, the endothelium must also be
ready to alter its membrane properties to allow white
blood cells to adhere and emigrate
in response to inflammation.
Atherosclerosis and blood clots may develop when the intimal lining
of a vessel is damaged.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
 Media
(tunica media)
Media
(tunica media)
The media is the middle layer of a blood vessel. In most arteries
and veins it is the thickest of the three tunics.
- The thickness of the media is generally proportional to the overall
diameter of the vessel.
 The media of arteries is generally thicker
than the media of veins of comparable diameter.
The media of arteries is generally thicker
than the media of veins of comparable diameter.
The media consists of smooth muscle and
elastic tissue in proportions which vary according to the type and size of vessel.
Elastic arteries have the highest proportion of elastic
tissue while muscular arteries have the highest proportion
of smooth muscle.
- In arteries a continuous layer of elastic
tissue, called the internal elastic lamina, marks the boundary
between the media and the intima.
- In most vessels, the smooth muscle fibers
are arranged circumferentially, so the plane of section across a vessel
can be deduced by the orientation/shape of smooth muscle nuclei.
 Elongated smooth muscle nuclei indicate longitudinally-cut
muscle fibers and hence a transversely-sectioned vessel.
Elongated smooth muscle nuclei indicate longitudinally-cut
muscle fibers and hence a transversely-sectioned vessel.- Tiny round smooth muscle nuclei indicate transversely-cut
muscle fibers and hence a longitudinally-sectioned vessel.
- (Curiously, veins in the adrenal medulla have bundles of smooth muscle arranged longitudinally.)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
 Adventitia
(tunica adventitia)
Adventitia
(tunica adventitia)
Ordinary fibrous connective tissue
forms the outer, adventitial layer of blood vessels, as it does for most tubular organs. This adventitial connective
tissue is usually more or less continuous with the stromal connective tissue
of the organ in which the vessel is found. That is, there is not a distinct
outer boundary to the tunica adventitia.
Nevertheless, the fibers of adventitial connective tissue tend to be more
concentric around the vessel and often somewhat denser than the surrounding
connective tissue (fascia). Tunica adventitia may also contain numerous elastin
fibers.
Clinical note: The presence of adventitial connective tissue
tightly adhering to vessels facilitates the surgical isolation and repair
of vessels.
TOP OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Arteries
The largest arteries, such as the aorta and its larger branches, have a tunica
media dominated by elastic tissue.
The elasticity conferred by elastin allows these elastic arteries to
smooth out the sharp changes in blood pressure resulting from the pumping
heart.
Most arteries are muscular arteries, with a
media dominated by smooth muscle. But
elastin is also a substantial component.
Arterioles
Arterioles are
the smallest arteries. Note that gross anatomists and surgeons
may use the term arteriole for any very small artery. Histologists
tend to use the term only for terminal arterial vessels
(i.e., those immediately preceding a capillary bed). Terminal (histological) arterioles are characterized
by having only a single layer of smooth
muscle cells.
Because smooth muscle fibers
are arranged circumferentially, the plane of section across an arteriole
can be inferred by the orientation/shape of smooth muscle nuclei.

- Elongated smooth muscle nuclei indicate longitudinally-cut
muscle fibers and hence a transversely-sectioned vessel.
- Tiny round smooth muscle nuclei indicate transversely-cut
muscle fibers and hence a longitudinally-sectioned vessel.
Most arteries have a continuous layer of elastin, called the internal elastic
lamina, at the boundary between the media and the
intima.
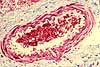
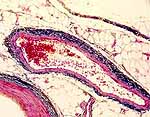
 In
routine histological sections, the internal elastic lamina of transversely-sectioned
arteries typically displays a distinctive sinusoidal appearance, resulting
from postmortem contraction of the artery's smooth muscle in the absence
of normal blood pressure.
In
routine histological sections, the internal elastic lamina of transversely-sectioned
arteries typically displays a distinctive sinusoidal appearance, resulting
from postmortem contraction of the artery's smooth muscle in the absence
of normal blood pressure.
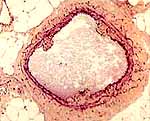
The thickness of arterial walls is typically not much less than the diameter
of the lumen. With such relatively thick walls, arteries tend to retain
a round cross-section in postmortem histological preparations (in contrast
to veins, which tend to appear more flattened).
Note that arteries of pulmonary
circulation (which convey blood of lower pressure than systemic circulation)
have relatively thinner walls, similar to systemic veins.
TOP OF
THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
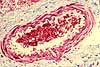
Veins
Veins have a wall similar to that of arteries
but with a thinner tunica media.
- The intima of a vein may fold inward at intervals to form valves such that blood can flow
only toward the heart.
Historical note: William
Harvey first recognized the function of valves in veins, which he described in his
de Motu Cordis, 1628. Harvey also described how these valves could be demonstrated
in an everyday classroom setting (see here).
- The walls of the smallest veins (sometimes called
"venules") do not include smooth
muscle.
The thickness of vein walls is typically much less than the diameter of the
lumen (i.e., proportionately much thinner than arteries carrying a similar
volume). With such relatively thin walls, veins tend to appear flattened
or collapsed in cross-section in postmortem histological preparations
(in contrast to arteries, which tend to appear more
round).
Note that vessels of pulmonary
circulation (which convey blood of lower pressure than systemic circulation)
have relatively thinner walls than systemic vessels of comparable diameter.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Capillaries and sinusoids
Capillaries and sinusoids are the smallest (microscopic) vessels, providing
communication between arteries
and veins.
Historical note: The existence of capillaries
was predicted by William
Harvey in 1628, as a necessary corollary of his theory of blood circulation.
Capillaries were actually observed in 1661 by Marcello
Malpighi using a newly invented instrument, the microscope.
For a more thorough account of historical understanding of capillaries, see
"The history of the capillary wall:
doctors, discoveries, and debates," by C. Hwa and W.C. Aird, in
Am J Physiol Heart Circ Physiol 293: H2667-H2679 (2007),
doi:10.1152/ajpheart.00704.
NOTE: In histological preparations, capillaries tend to be quite inconspicuous
unless they contain red blood cells. Capillary endothelial nuclei are seldom close together and
are commonly difficult to distinguish from fibroblasts and other connective
tissue cells, unless the preparation is fine enough to resolve the thin
endothelial cytoplasm surrounding a small lumen.
Historical note: Ignoring
inconspicuous tissue features such as capillaries can have consequences. Since stromal capillaries
are seldom evident in tissue specimens, they are often ignored and forgotten. Unfortunately,
just such inattention may have delayed for decades the realization that
interfering with tumor vasculature might powerfully inhibit tumor growth.



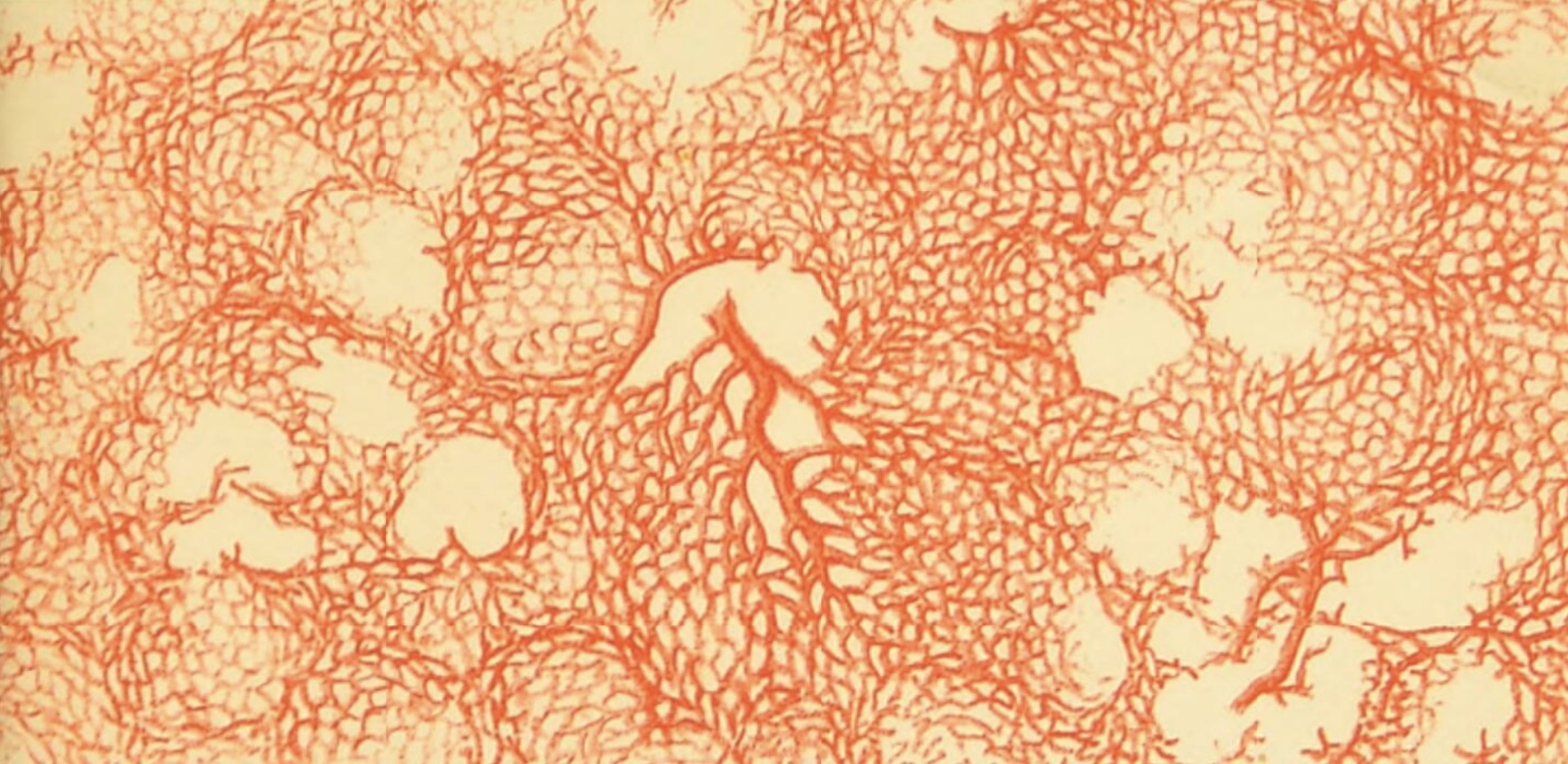
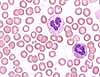
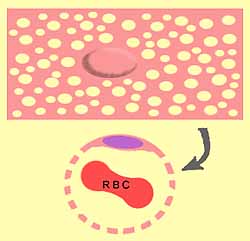
By definition, capillaries are vessels whose diameter is so small (less
than 10µm) that red blood cells must pass through in single file (thumbnail
at left).
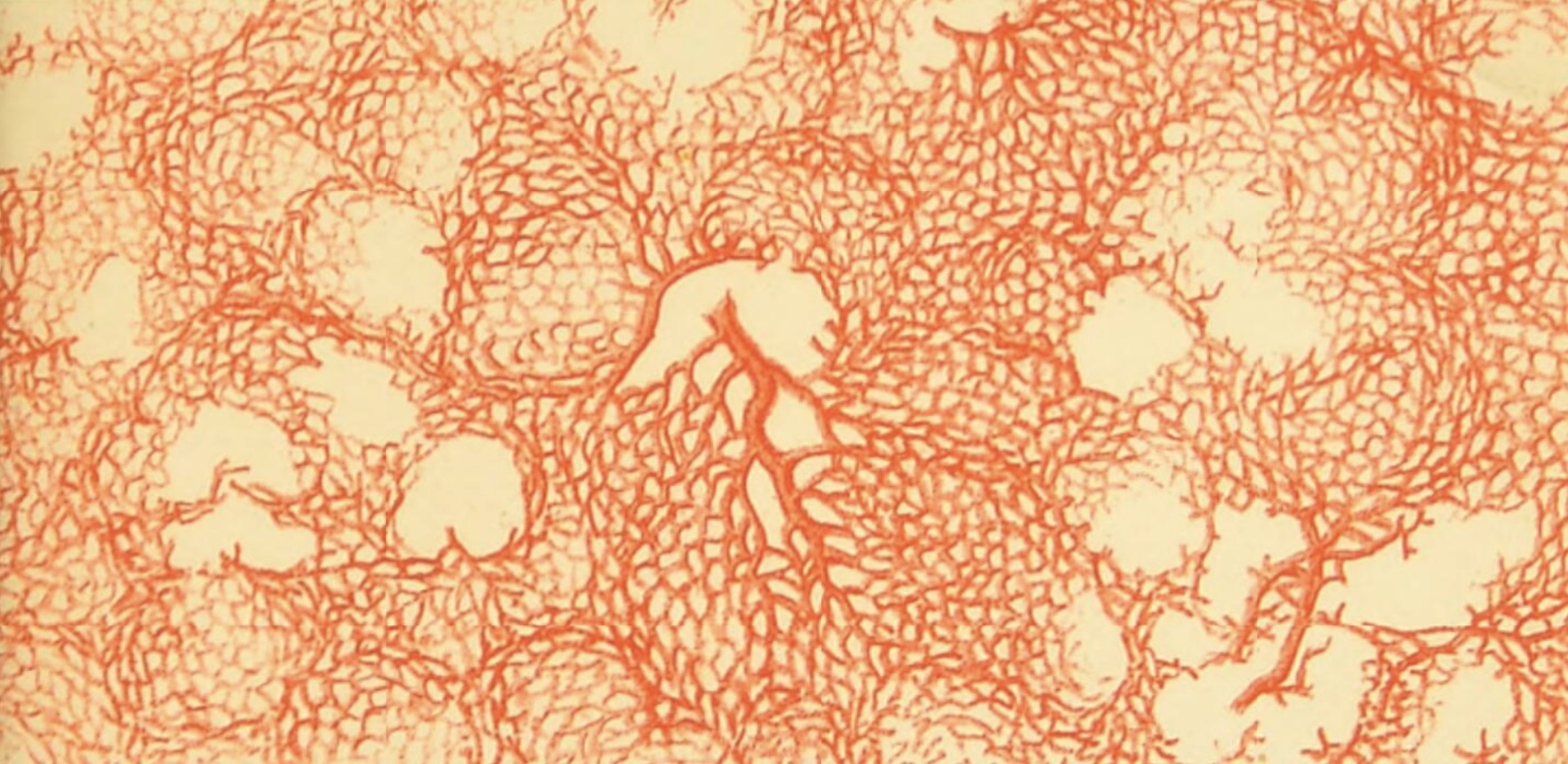
Capillaries often form an interconnected plexus, or "capillary bed."
Thumbnails at right show capillaries within lung, kidney and stomach.
In contrast to capillaries, sinusoids are typically more voluminous
(for an example, see liver).
Although the lumen of a sinusoid is commonly narrow in one dimension, it may
be extensive in another dimension, like an alley-way space between the walls of adjacent buildings rather
than the hollow of a tube.
 The
walls of capillaries and sinusoids consist of little more than endothelium.
A single thin, flattened endothelial cell forms a segment of capillary, like
a sheet of paper rolled into a tube (with a small bulge at the site of the
nucleus). These single-cell tubes are then attached end-to-end to form
a capillary.
The
walls of capillaries and sinusoids consist of little more than endothelium.
A single thin, flattened endothelial cell forms a segment of capillary, like
a sheet of paper rolled into a tube (with a small bulge at the site of the
nucleus). These single-cell tubes are then attached end-to-end to form
a capillary.
Wrapped at intervals around capillaries are pericytes (originally called Rouget cells,
after C.M.B. Rouget, b. 1824),
cells with contractile properties that can apparently adjust capillary blood
flow. This effect has been demonstrated for local microvascular control
of blood flow in the brain.
Research notes:
MacVicar & Salter, Neuroscience:
Controlled capillaries, Nature 443, 642-643 (12 October 2006)
| doi.org/10.1038/443642a.
Dore-Duffy & Cleary, Morphology and properties of pericytes,
Methods in Molecular Biology, vol. 686, pp. 49-68 (2011)
| doi.org/10.1007/978-1-60761-938-3_2.
Sweeney, Ayyadurai & Zlokovic, Pericytes of the neurovascular unit: key functions and signaling pathways.
Nature Neuroscience 19, 771-783 (2016) | doi.org/10.1038/nn.4288.
In most parts of the body, capillaries and sinusoids are more or less "leaky."
The degree of "leakiness" is determined by variations in
the endothelial lining of the capillaries.
- In most ordinary connective tissue, adjacent endothelial cells are incompletely
sealed together.
- In many visceral organs, notably the kidney
and the liver, each endothelial
cell is full of patent holes called fenestrations (L., windows).
- In the brain and a few other places, endothelial cells are closely attached
to one another, forming a tight seal so that any transfer of materials can
occur only by passing across the endothelial cells (i.e., crossing endothelial
membranes and cytoplasm).
In ordinary connective tissue, plasma leakage is typically balanced by re-absorption
and/or lymph drainage. A shift in the balance (e.g., increased vascular
permeability due to inflammation) can result in accumulation of tissue fluid,
or edema.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Heart
The lining of the heart is similar to that of blood vessels, with an intima
including endothelium.
The pericardium (the heart's outer surface) is a serosa lined by mesothelium.
Mesothelium -- a simple squamous
epithelial tissue, derived from mesoderm -- forms the surface lining
not only the pericardial cavity but also peritoneal and pleural cavities
(i.e., all major body cavities).
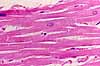
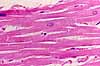
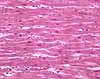
 The bulk of the heart consists of cardiac muscle, one of the three distinct
types of muscle in the body. (The other two muscle types are skeletal
muscle and smooth muscle.)
The bulk of the heart consists of cardiac muscle, one of the three distinct
types of muscle in the body. (The other two muscle types are skeletal
muscle and smooth muscle.)
|
Compare muscle fiber types
|
|
|
|
|
|
Cardiac muscle
|
|
|
Cardiac pathology
yields characteristic changes in the structure/appearance of cardiac muscle.
Cardiac muscle has several
distinct characteristics.
- Cardiac muscle is striated, like skeletal
muscle. (For brief description of striations, see skeletal
muscle.)
- Cardiac muscle consists of distinct, individual cells (unlike skeletal
muscle which consists of immensely long, multinucleate fibers).
- Cardiac muscle cells are attached end-to-end by specialized junctions
called intercalated discs.
 Intercalated discs consist of adhering junctions (into which
the contractile myofilaments are attached) and gap junctions (which
allow passage of ions thereby establishing electrical connection between
adjacent cells.)
Intercalated discs consist of adhering junctions (into which
the contractile myofilaments are attached) and gap junctions (which
allow passage of ions thereby establishing electrical connection between
adjacent cells.)
 Intercalated
discs appear pale in routine H&E
stained sections but may be highlighted by special stains.
Intercalated
discs appear pale in routine H&E
stained sections but may be highlighted by special stains.
For detailed images of intercalated discs, see the
Electron Microscopic Atlas of cells, tissues and organs in the internet:
- Each end of a cardiac muscle cell may attach to two or more other
cells, so that the fibrous structure of cardiac muscle appears to be branched
(unlike skeletal muscle, where each fiber
is a single, discrete unit).
For more information about cardiac muscle cells, see your
textbook.
For more electron micrographs of heart muscle, see the Electron Microscopic Atlas of cells, tissues and organs in the internet.
 Specialized cardiac muscle cells form bands called Purkinje fibers
(named after Johann Purkinje, b. 1787), which conduct
electrical signals to coordinate heart contractions (see your physiology resources).
Purkinje fibers have a larger diameter and paler cytoplasm (i.e., fewer
contractile filaments) than ordinary cardiac muscle fibers. Both of
these features are adaptations for reducing electrical resistance and increasing
the speed of electrical conduction.
Specialized cardiac muscle cells form bands called Purkinje fibers
(named after Johann Purkinje, b. 1787), which conduct
electrical signals to coordinate heart contractions (see your physiology resources).
Purkinje fibers have a larger diameter and paler cytoplasm (i.e., fewer
contractile filaments) than ordinary cardiac muscle fibers. Both of
these features are adaptations for reducing electrical resistance and increasing
the speed of electrical conduction.
See WebPath
Myocardial Infarction for description and images of cardiac pathology.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Lymphatic System
The lymphatic system consists of:
The lymphatic system serves two principal functions.
- The lymphatic system provides a route for excess interstitial fluid ("lymph")
to return to the blood.
- The lymphatic system provides the means for immune system cells (most
notably lymphocytes) to travel,
communicate, and proliferate; thus the lymphatic system is instrumental
in the process of immunological defense, including inflammation.
(Continue down this page for additional introductory material. However, an in-depth treatment of the immune system is beyond the scope of this website.)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Lymphatic vessels
Lymphatic vessels (often just called lymphatics) are channels
which drain excess fluid ("lymph") from tissues.
In most peripheral tissues, some plasma seeps out of capillaries.
A portion of this is taken back up in venules while the rest drains into
terminal lymphatic channels, also called lymphatic capillaries. A
shift in the balance between fluid entering and leaving tissues (e.g., increased
vascular permeability due to inflammation) can result in accumulation of
tissue fluid, or edema.
All lymphatic vessels eventually lead "downstream"
to the thoracic duct, which empties into the vena cava (a point where blood
pressure is quite low; higher pressure would impede drainage).
Directional flow in lymphatic vessels is maintained by Swammerdam valves
(commemorating Jan Swammerdam, b. 1637).
Lymphatic vessels resemble blood vessels with exceptionally delicate
walls (and, of course, without red blood cells). Smaller lymphatic vessels
consist of little more than endothelium.
If, while examining a histological specimen, you encounter
a flattened, endothelially-lined passage that seems too delicate to be a
vein but too large to be a capillary, it is probably a lymphatic.
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Lymph nodes and nodules

 Lymph
nodes are small organs, found in scattered locations along the lymphatic
drainage system of the body.
Lymph
nodes are small organs, found in scattered locations along the lymphatic
drainage system of the body.
Some lymph nodes can be palpated, where they are sometimes
called "glands," especially when swollen in reaction to infection.
Lymph nodes provide "gathering places" through which wandering
lymphocytes must pass as they travel from peripheral
tissues on their return to systemic circulation. Within the lymph nodes,
activated lymphocytes (i.e., those
which have encountered an antigen which they recognize) proliferate, producing
more lymphocytes able to respond
to the same antigen.
Metaphorically, lymph nodes might be considered to be "filters"
for peripheral interstitial fluid.
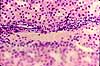
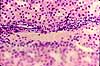
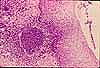
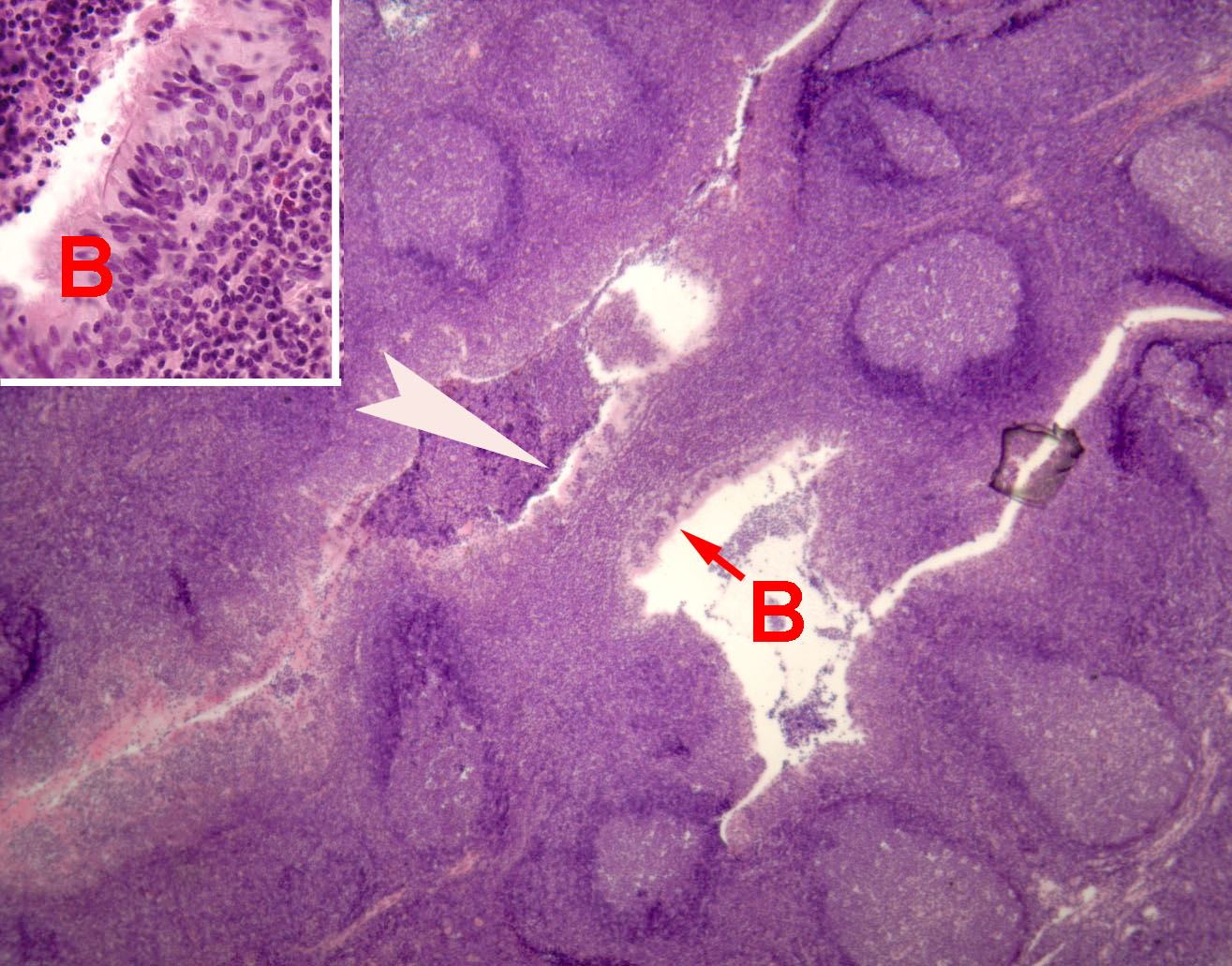
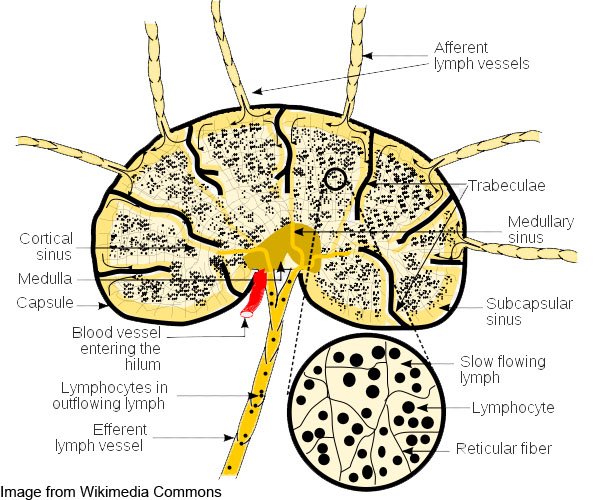
 Lymph nodes consist of a fibrous connective tissue capsule enveloping many lymphocytes
and other immune-system cells, into and through which lymph flows (diagram).
The parenchyma of a lymph node is organized into cortex and
medulla. In the cortex, lymphocytes are gathered into lymph nodules,
also called lymphoid follicles, which are sites where lymphocytes
congregate. At the center of each lymph nodule is a germinal center
where lymphocytes proliferate.
Lymph nodes consist of a fibrous connective tissue capsule enveloping many lymphocytes
and other immune-system cells, into and through which lymph flows (diagram).
The parenchyma of a lymph node is organized into cortex and
medulla. In the cortex, lymphocytes are gathered into lymph nodules,
also called lymphoid follicles, which are sites where lymphocytes
congregate. At the center of each lymph nodule is a germinal center
where lymphocytes proliferate.
Lymph nodules cluster toward the cortex of the lymph node, where afferent lymph
vessels pass through the capsule. The medulla appears less visibly organized. An efferent lymph vessel
drains the lymph node from the hilus, in the region of the medulla (diagram). A lymph node also receives
circulating blood coming in through the hilus and passing through "high endothelial
venules, specialized for interacting with the lymphocytes.
 Lymph nodes are supported within by a network of reticular
fibers.
Lymph nodes are supported within by a network of reticular
fibers.
 For additional information, see your text.
For additional information, see your text.
Key for microscopic differentiation
of lymphoid tissues (courtesy M. O'Keefe, MSI)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Mucosa-associated lymphoid tissue ("MALT") and Gut-associated lymphoid tissue ("GALT")
Lymphoid tissue occurs in lamina propria of most mucosal organs, where it is sometimes referred to as MALT (Mucosa-Associated
Lymphoid Tissue), most conspicuously
in the gastrointestinal tract, where it
is sometimes referred to as GALT (Gut-Associated Lymphoid Tissue).
 The most characteristic features of mucosa-associated lymphoid tissue are lymph
nodules, also called lymphoid follicles, which are sites where
lymphocytes congregate. At
the center of each lymph nodule is a germinal center where the lymphocytes
proliferate.
The most characteristic features of mucosa-associated lymphoid tissue are lymph
nodules, also called lymphoid follicles, which are sites where
lymphocytes congregate. At
the center of each lymph nodule is a germinal center where the lymphocytes
proliferate.
 The connective tissue around a lymph nodule is usually heavily infiltrated with
lymphocytes migrating to and from
the germinal center.
The connective tissue around a lymph nodule is usually heavily infiltrated with
lymphocytes migrating to and from
the germinal center.
 Lymph nodules may occur in lamina propria
anywhere along the GI tract. Large aggregations of lymph nodules may
extend beyond lamina propria and intrude into the submucosa. Nearby
epithelial tissue may also be infiltrated by lymphocytes.
Lymph nodules may occur in lamina propria
anywhere along the GI tract. Large aggregations of lymph nodules may
extend beyond lamina propria and intrude into the submucosa. Nearby
epithelial tissue may also be infiltrated by lymphocytes.

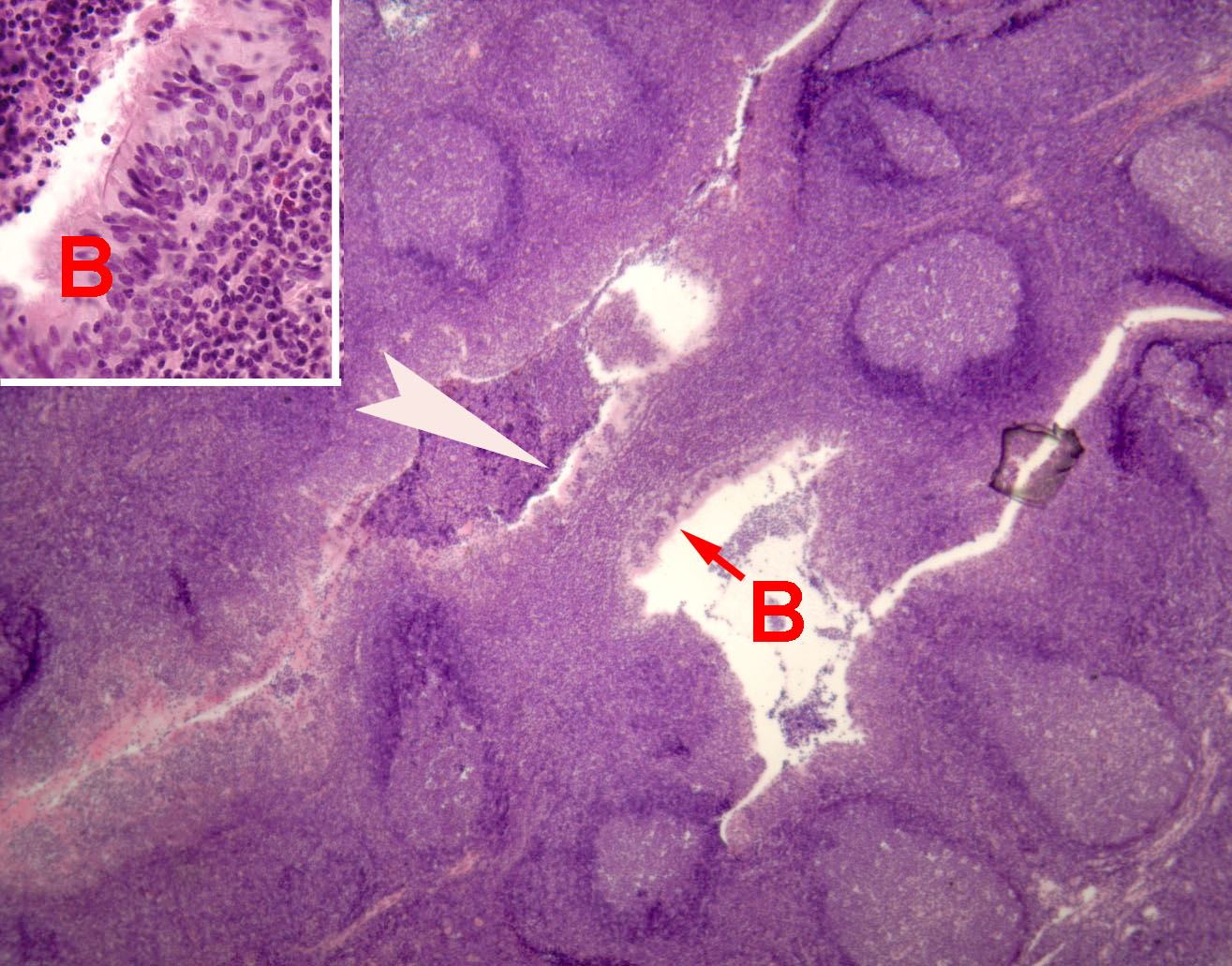 Aggregations of lymph nodules are characteristic of tonsils,
Peyer's patches, and appendix.
Aggregations of lymph nodules are characteristic of tonsils,
Peyer's patches, and appendix.
For more on MALT, consult your histology text.
Key for microscopic differentiation
of lymphoid tissues (courtesy M. O'Keefe, MSI)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Spleen

 The spleen is an organ in which lymphoid tissue and blood are intermixed
and served by a network of vascular sinusoids. The loose lymphoid and
blood cells are contained within a fibrous connective tissue capsule and supported
by strands of fibrous connective tissue ("trabeculae"). Lymphoid
tissue forms the so-called "white pulp" while surrounding tissue
rich in blood forms "red pulp."
The spleen is an organ in which lymphoid tissue and blood are intermixed
and served by a network of vascular sinusoids. The loose lymphoid and
blood cells are contained within a fibrous connective tissue capsule and supported
by strands of fibrous connective tissue ("trabeculae"). Lymphoid
tissue forms the so-called "white pulp" while surrounding tissue
rich in blood forms "red pulp."
The spleen is enclosed by a tough capsule of dense collagenous
connective tissue. Arteries enter the capsule, extend some distance into the body of the spleen
where they tend to be surrounded by white pulp, and then open into sinusoids in the capsular space.
So, circulation within the spleen is essentially open, unconstrained by capillaries or veins.
Leaving the spleen, a portal vein carries blood to the liver.
The color names for red and white pulp reflect their natural
(unstained) color, with red pulp colored by red blood cells while white
pulp takes on the creamy color of massed lymphocytes (similar to pus).
For more detailed description of spleen structure and function, consult your
text.
Key for microscopic differentiation
of lymphoid tissues (courtesy M. O'Keefe, MSI)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.
Thymus
 The thymus is the primary organ for maturation of lymphocytes. It plays
a central role in developing self-tolerance (i.e., the immune system's ability
to avoid attacking the body's own cells). "Promiscuous gene expression"
in stromal epithelial cells of the thymus leads to deletion of T-cells that react to self-antigen.
(A similar process has been detected in peripheral lymph nodes; see
Science
321:776, 8 August 2008.)
The thymus is the primary organ for maturation of lymphocytes. It plays
a central role in developing self-tolerance (i.e., the immune system's ability
to avoid attacking the body's own cells). "Promiscuous gene expression"
in stromal epithelial cells of the thymus leads to deletion of T-cells that react to self-antigen.
(A similar process has been detected in peripheral lymph nodes; see
Science
321:776, 8 August 2008.)

 Superficially, the thymus resembles a gland subdivided into numerous small lobules.
But the thymus has no ducts and no proper secretory tissue. In an active
(i.e., young) thymus, the cortex of each lobule is densely packed with lymphocytes while
each lobule has a paler medullary core where cells are dividing. The thymus
also contains cells called "reticular cells," "epitheliocytes,"
"dendritic cells," and "stromal cells." Although
such cells are generally inconspicuous in routine histological specimens,
clusters may be evident as "Hassall's corpuscles"
(commemorating Arthur
Hassall, b. 1817).
Superficially, the thymus resembles a gland subdivided into numerous small lobules.
But the thymus has no ducts and no proper secretory tissue. In an active
(i.e., young) thymus, the cortex of each lobule is densely packed with lymphocytes while
each lobule has a paler medullary core where cells are dividing. The thymus
also contains cells called "reticular cells," "epitheliocytes,"
"dendritic cells," and "stromal cells." Although
such cells are generally inconspicuous in routine histological specimens,
clusters may be evident as "Hassall's corpuscles"
(commemorating Arthur
Hassall, b. 1817).
Research news: Hassall's corpuscles have been associated with the processes of T cell
selection. See, e.g., Nature 436: 1181-1185; (2005).
For more information on thymus structure and function, consult your text.
Key for microscopic
differentiation of lymphoid tissues (courtesy M. O'Keefe,
MSI)
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE / CARDIOVASCULAR IMAGE INDEX.


 Cardiovascular pathology
Cardiovascular pathology
WebPath
offers an extensive image collection for blood
and bone marrow smears, both normal and pathological.
WebPath
also provides a tutorial
on myocardial infarction and an extensive set of images associated with
atherosclerosis.
Note especially the following specific examples
TOP
OF THIS PAGE / CONTENTS
FOR THIS PAGE
Image index
TOP OF THIS PAGE / CONTENTS
FOR THIS PAGE
 Comments
and questions: dgking@siu.edu
Comments
and questions: dgking@siu.edu
SIUC / School
of Medicine / Anatomy / David
King
https://histology.siu.edu/crr/cvguide.htm
Last updated: 10 May 2025 / dgk
 Histology Study Guide
Histology Study Guide


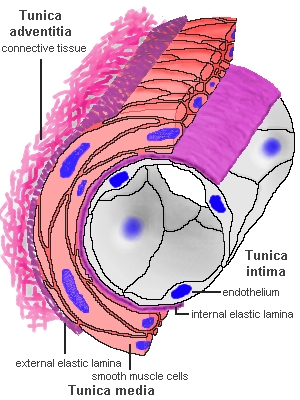 Histologically,
blood vessels consist of concentric layers or "tunics"
of different tissue types.
Histologically,
blood vessels consist of concentric layers or "tunics"
of different tissue types.

































 Comments
and questions:
Comments
and questions: