Specialized Cells of
the GI System
The GI system includes a number of highly specialized cell types, each differentiated
to perform a specific function.
Most of the listed cells are epithelial, since variously
specialized epithelia carry out most of the functions which are specific
to the GI system. Other tissues are also vitally important to GI function,
but are basically similar in all organ systems and are not individually
listed here. See separate pages for smooth
muscle, for cells of connective tissue
(including immune system), and for nerve
cells.
Listing of Cells by Region
Listing of Cells by Function
Listing of Cells by Name
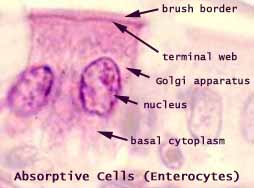
Intestinal Absorptive Cells
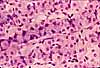
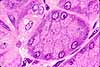
Absorptive cells, or enterocytes, are the predominant epithelial
cell type lining the lumen of the small intestine
and colon. These cells are specialized for absorption
of nutrients across the apical plasma membrane and export of these same nutrients
across the basal plasma membrane. Upon release at the basal end of the
cell, nutrient molecules diffuse into connective tissue space and eventually
into capillaries or lacteals of the lamina
propria.
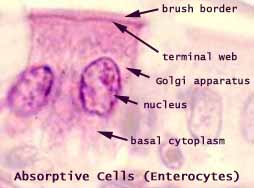 The
apical surface area of each absorptive cell is greatly increased by
evagination into a dense array of microvilli, visible microscopically
as the brush border.
The
apical surface area of each absorptive cell is greatly increased by
evagination into a dense array of microvilli, visible microscopically
as the brush border.
In the small intestine, brush
border enzymes contribute to digestive breakdown (these enzymes are lacking
from absorptive cells of the colon).
The microvilli are supported by an underlying meshwork
of microfilaments which comprise the terminal web. At the lateral
edges of each cell, the the terminal web reinforces the junctional complex
that attaches adjoining cells. (This site is sometimes visible microscopically
as a terminal bar at the apical corners of each cell.)
A pale (poorly stained) region above the nucleus indicates
the location of the Golgi apparatus, where some absorbed nutrients
are processed for transport.
Associated cell types: Interspersed among
the many absorptive cells of the intestinal epithelium are scattered goblet
cells, occasional enteroendocrine cells (which
are difficult to distinguish in routine preparations), and occasional wandering
cells of the immune system (e.g., lymphocytes, eosinophils).
 The
life-span of absorptive cells is short, only a few days. During
this time, the cells migrate from deep in crypts, where they are formed by
dividing stem cells, to the surface epithelium where they
eventually undergo apoptosis. Along villi, this migration is sometimes
called "the epithelial escalator." Look for apoptosis at
the tips of villi.
The
life-span of absorptive cells is short, only a few days. During
this time, the cells migrate from deep in crypts, where they are formed by
dividing stem cells, to the surface epithelium where they
eventually undergo apoptosis. Along villi, this migration is sometimes
called "the epithelial escalator." Look for apoptosis at
the tips of villi.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
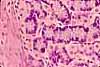
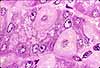
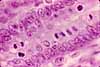
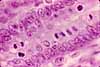
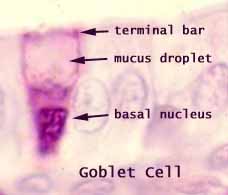
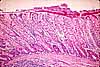
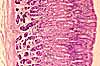
Goblet cells
Goblet cells are scattered among the absorptive
cells in the epithelium of the small intestine
and colon. These epithelial cells are specialized
for secretion of mucus, which facilitates passage of material through the
bowel. The name "goblet" refers to the cell's shape, narrow
at the base and bulging apically.
(Visually similar cells, also called "goblet cells," are found in the respiratory and
reproductive tracts.)
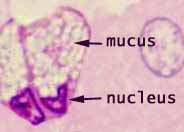
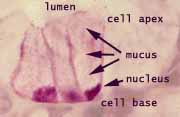
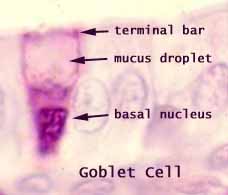 The
apical end of each goblet cell is occupied by a large mass of mucus,
which compresses adjacent cells (thus conferring the characteristic "goblet"
shape) and displaces the nucleus toward the basal end of the cell. As
in other mucous cells, the nucleus is compact and intensely-stained.
The
apical end of each goblet cell is occupied by a large mass of mucus,
which compresses adjacent cells (thus conferring the characteristic "goblet"
shape) and displaces the nucleus toward the basal end of the cell. As
in other mucous cells, the nucleus is compact and intensely-stained.
Goblet cells comprise an integral part of the epithelium, attached
by junctional complexes (evidenced in light microscopy as the "terminal
bar") to adjacent absorptive cells.
The proportion of goblet cells to absorptive cells
increases along the entire length of the bowel, with relatively few in the
duodenum and very many in the colon.
The colonic epithelium gives the superficial impression of being almost
entirely goblet cells, but there are still several times as many absorptive
cells. The goblets are just more conspicuous, with their bulging mucus
droplets.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
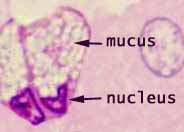
Mucous cells
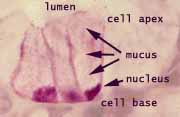 Epithelial
cells which are specialized to secrete mucus are called mucous
cells. In routine light microscopy, mucous
cells are most conspicuously distinguished by their "empty"
appearance (i.e., poorly stained cytoplasm) and densely-stained, basal nuclei.
Epithelial
cells which are specialized to secrete mucus are called mucous
cells. In routine light microscopy, mucous
cells are most conspicuously distinguished by their "empty"
appearance (i.e., poorly stained cytoplasm) and densely-stained, basal nuclei.
The nucleus in a typical mucous cell gives the impression
of having been displaced and compressed by the mass of mucus accumulated
in the apical end of the cell.
Mucus does not stain well with standard acidic or basic
dyes, but is demonstrated with the Periodic Acid Shiff
procedure (PAS stain).
 Examples
of mucous cells in the GI may be found in salivary glands,
esophageal glands, stomach
surface, and Brunner's glands of the duodenum.
Goblet cells are mucous cells which are scattered individually within
a columnar epithelium; these are a characteristic feature of the intestine
(as well as the respiratory tract and the female reproductive tract).
Examples
of mucous cells in the GI may be found in salivary glands,
esophageal glands, stomach
surface, and Brunner's glands of the duodenum.
Goblet cells are mucous cells which are scattered individually within
a columnar epithelium; these are a characteristic feature of the intestine
(as well as the respiratory tract and the female reproductive tract).
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
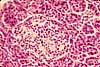
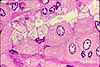
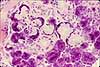
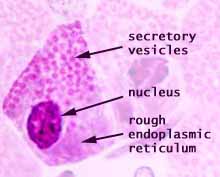
Serous Cells
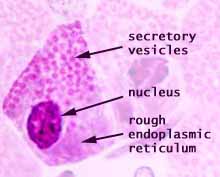 Serous
cells, exemplified by pancreatic acinar cells, are glandular epithelial
cells specialized for exocrine enzyme secretion.
Serous
cells, exemplified by pancreatic acinar cells, are glandular epithelial
cells specialized for exocrine enzyme secretion.
A serous cell's cytoplasm is visibly polarized, with basophilic basal
cytoplasm and variously-staining secretory vesicles (zymogen granules)
concentrated in apical cytoplasm. The basal basophilia is due to a concentration
of protein synthetic organelles (ribosomes on rough endoplasmic
reticulum). The Golgi apparatus is usually located midway
along the cell, typically in a supranuclear position.
Examples of serous cells include acinar
cells of pancreas and salivary
glands, gastric chief cells, and intestinal Paneth
cells.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
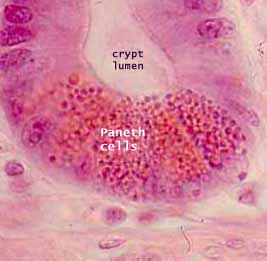
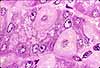
Paneth cells
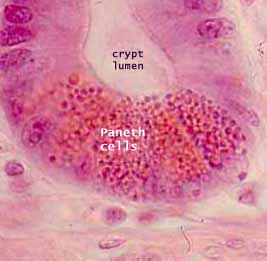 Paneth
cells (named for Joseph Paneth, b. 1857) are secretory epithelial cells located at the ends of intestinal
crypts. The function for these cells
is secretion of anti-bacterial proteins into the crypt lumen, thereby providing
protection for the stem cells which line the crypt walls.
Paneth
cells (named for Joseph Paneth, b. 1857) are secretory epithelial cells located at the ends of intestinal
crypts. The function for these cells
is secretion of anti-bacterial proteins into the crypt lumen, thereby providing
protection for the stem cells which line the crypt walls.
For relatively recent research concerning the protective functions
of Paneth cells and intestinal mucus, see Science 334:182
(14 October 2011), "Keeping bacteria at a distance."
Paneth cells have typical serous-secretory
appearance, with basophilic basal cytoplasm (containing protein-synthetic
rough endoplasmic reticulum) and apical secretory vesicles (zymogen granules).
The secretory vacuoles of Paneth cells contain lysosomal enzymes,
with anti-bacterial function.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Myoepithelial cells
Myoepithelial cells are contractile epithelial cells which forcibly
express the contents of a gland. Although myoepithelial
cells function like smooth muscle, they are typically
located within a glandular epithelium, between the secretory cells and the
basement membrane. Each myoepithelial cell has long cytoplasmic processes
which wrap around a secretory unit. Hence, contraction of the myoepithelial
processes can squeeze secretory product from the secretory unit into its duct.
 Myoepithelial
cells contribute significantly to the secretory activity of sweat
glands, salivary glands, and mammary
glands.
Myoepithelial
cells contribute significantly to the secretory activity of sweat
glands, salivary glands, and mammary
glands.
In routine histological preparations, myoepithelial cells
are inconspicuous. The cell body can sometimes be noticed as an "extra"
nucleus beneath some secretory cells. The contractile process are
thin eosinophilic strands. In routine H&E stained sections of
sweat glands, these can often be seen as small pink triangles underlying
the secretory cells. In sweat glands
and mammary glands, myoepithelial processes are
normally difficult to observe without special stains.
- For myoepithelial cells in breast tissue, see WebPath.
Consult your histology textbook and/or atlas for additional
detail and micrographs of these cells.
 Taste
Cells
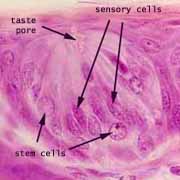
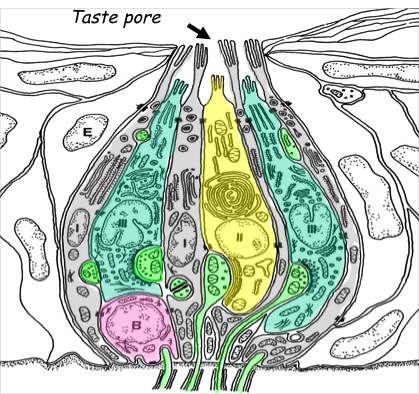
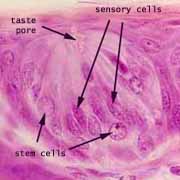
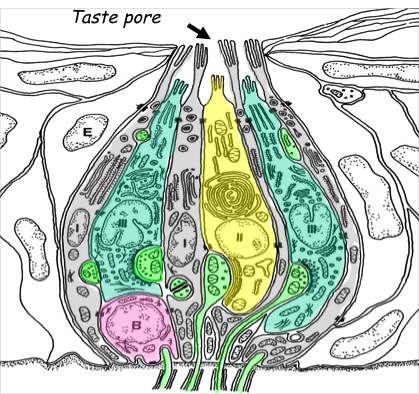
Taste
Cells
The sensation of taste is mediated by columnar epithelial sensory
cells which occur in clusters called taste
buds on fungiform and circumvallate
papillae of the tongue. Taste buds
interrupt and extend across the tongue's stratified squamous epithelium.
These sensory cells are normally replaced every 10-14 days
by division and differentiation of stem cells,
which is handy since they are exposed and easily damaged (e.g., by a bite
of too-hot pizza).
Associated cell types: In addition to sensory
cells, the elongated cells of the taste bud include support cells,
which are sometimes (rather pretentiously) called sustentacular cells
(from the same root as "sustain"). Stem
cells are normally visible in taste buds as shorter cells with round nuclei
which appear at the basal end of the tastebud.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells
 |
|
 |
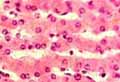
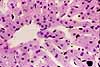
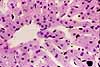
Hepatocytes
Although all cells are general-purpose metabolic factories,
most mature cell types are functionally specialized to play one particular
role in the economy of the larger body. In contrast, hepatocytes
of the liver are remarkable for the breadth
of their "specialization." Among other functions,
hepatocytes:
- form and secrete bile
- store glycogen and buffer blood glucose
- synthesize urea
- metabolize cholesterol and fat
- synthesize plasma proteins
- detoxify many drugs and other poisons
- process several steroid hormones and vitamin D
The cellular structure of hepatocytes is correspondingly
rich. Instead of displaying a concentration of one particular organelle,
hepatocytes have lots of everything -- lots of mitochondria, lots of
ribosomes, lots of Golgi bodies, lots of endoplasmic reticulum
(both rough and smooth), lots of stored glycogen, lots of lysosomes,
lots of plasma membrane (with microvilli on the free surface).
They even have lots of nucleus (yes, hepatocytes may be polyploid
and commonly have two full-size nuclei).
When an introductory biology book illustrates "the
cell," the representative example is often a hepatocyte -- because
hepatocytes offer splendid and numerous examples of most cellular organelles.
 In appearance, hepatocytes are boxy (cuboidal) cells with one or two large
euchromatic nuclei and with abundant, grainy cytoplasm that stains well with
both acid and basic dyes (reflecting the abundance of various cellular constituents).
Because individual liver cells have an indefinite lifespan, they may
accumulate abundant lipofuscin (yellow-brown
"wear-and-tear" pigment), especially with advancing age.
In appearance, hepatocytes are boxy (cuboidal) cells with one or two large
euchromatic nuclei and with abundant, grainy cytoplasm that stains well with
both acid and basic dyes (reflecting the abundance of various cellular constituents).
Because individual liver cells have an indefinite lifespan, they may
accumulate abundant lipofuscin (yellow-brown
"wear-and-tear" pigment), especially with advancing age.
 Hepatocytes are arranged into cords, in which each
hepatocyte is attached to its neighbors in a two-dimensional sheet. On
either side of the cord, each hepatocyte faces the space
of Disse, across which it communicates freely with adjacent sinusoids.
Hepatocytes are arranged into cords, in which each
hepatocyte is attached to its neighbors in a two-dimensional sheet. On
either side of the cord, each hepatocyte faces the space
of Disse, across which it communicates freely with adjacent sinusoids.
Hepatocytes are epithelial, but their epithelial nature is expressed
in a rather peculiar way.
An ordinary epithelial cell
sits on its basal surface, has an apical surface exposed to the external
space, and is attached to its neighbors along its lateral surface. In
principle, hepatocytes follow this same plan -- but
they have a unique topology.
 A
typical hepatocyte has two basal surfaces (deep orange in cartoon at right).
These two surfaces are found on opposite ends of the hepatocyte, where the cell faces the sinusoids
on either side of the cord in which it resides. These surfaces are characterized by microvilli,
which increase surface area for interaction with fluid in the space
of Disse.
The apical surface of a hepatocyte (green in the cartoon at right) occurs along
a narrow band around the cell's middle, half-way between the opposing basal surfaces.
It is across this surface that bile is secreted. The edges
of this apical surface are attached by junctional complexes to those of adjacent
hepatocytes, thereby forming the bile canaliculi.
A
typical hepatocyte has two basal surfaces (deep orange in cartoon at right).
These two surfaces are found on opposite ends of the hepatocyte, where the cell faces the sinusoids
on either side of the cord in which it resides. These surfaces are characterized by microvilli,
which increase surface area for interaction with fluid in the space
of Disse.
The apical surface of a hepatocyte (green in the cartoon at right) occurs along
a narrow band around the cell's middle, half-way between the opposing basal surfaces.
It is across this surface that bile is secreted. The edges
of this apical surface are attached by junctional complexes to those of adjacent
hepatocytes, thereby forming the bile canaliculi.
Bile canaliculi within each hepatic cord form a network encircling each hepatocyte.
(If the network were filled in, its shape would resemble chicken-wire, with
each ring of wire encircling one hepatocyte.) Along this network of tiny channels, bile can seep toward the periphery
of the lobule and hence into the proper bile ducts which are found only
portal areas. These ducts form the biliary tree which eventually exits the liver.
As bile canaliculi approach the portal area at the edge of a lobule, they merge into short channels
called canals of Hering (commemorating Ewald Hering,
b. 1834) lined by both hepatocytes and bile duct cells.
Bile canaliculi are barely visible in routine
microscopic preparations, at sites where the boundary between adjacent
hepatocytes has been cut neatly and perpendicularly. They can be
clearly demonstrated with special stains.
The lateral surfaces of a hepatocyte (pale orange in cartoon at right) take the form
of two broad bands which wrap around the cell between the two basal surfaces,
separated by the narrow band of apical surface. These lateral surfaces
attach the cell to its neighbors within the cord,
with junctional complexes sealing off and separating the bile canaliculi
(at the apical surface) from the plasma-containing space
of Disse (at the basal surfaces).
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Cautionary note: Some otherwise excellent textbooks
(as well as a distressingly high proportion of websites) misrepresent the three-dimensional
configuration of bile canaliculi within hepatic cords. The usual error
is to diagram canaliculi as if they were sandwiched between two layers of hepatocytes;
in fact, each cord is only one cell thick, with a canaliculus encircling each hepatocyte.
Endothelial Cells
Endothelial cells are simple squamous cells which line the entire
vascular system (including lymphatic
channels). For additional information (besides what appears here below),
see endothelium in the CRR Unit.
Endothelial cytoplasm is inconspicuous in routine light microscopy.
Typically only the nuclei are visible, at the boundary between the lumen
and the wall of a vessel. Endothelial nuclei typically appear thin and dark, in cross
section. However, occasionally endothelium lies parallel to the plane
of section. In this case the nuclei may appear very large, round,
and pale.
Historical note The obsoletle term reticuloendothelial system refers
to the macrophages of the liver,
spleen and lymph
nodes (i.e., those organs with elaborate endothelially-lined channels
supported by reticular connective tissue).
The name reflects former confusion about the distinction between endothelial
cells and the scattered population of macrophages (monocytes, histiocytes).
Macrophages can be readily labelled experimentally through their phagocytosis
of injected carbon particles. However, endothelial cells are also
labelled by the same procedure. Although endothelial cells are not
dramatically phagocytotic, they do shuttle some materials across the endothelial
lining via small endocytotic and exocytotic vesicles.
Although endothelial cells appear rather uninteresting under the microscope,
these are important cells. They are situated at a critical location,
between the blood and all other body cells. They secrete substances
which control local blood flow and blood coagulation, and they are active
participants in white blood cell emigration during inflammation.
Continuous endothelium. Throughout much of the body, the capillary
endothelial lining is continuous, with neither large gaps between cells
nor holes through cells. Materials pass through the endothelium either
by diffusion or via rapid vesicular transcytosis. (In most of the brain,
a lack of transcytotic vesicles accounts for the blood brain barrier -- the
only substances which cross such a barrier are those which can diffuse through
plasma membranes or those for which specific membrane channels exist.)
Fenestrated endothelium. In a few special locations -- notably
in the sinusoids of the liver, in
villi of the small intestine, in the glomeruli
of the kidney, and in most endocrine glands -- the
endothelium is fenestrated (i.e., full of holes -- from fenestra,
window). In the liver, where there is also no basement membrane, the
fenestrations permit blood plasma to wash freely over the exposed surfaces
of the hepatocytes through the space
of Disse.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Kupffer Cells (Liver Macrophages)
Kupffer cells (named after Karl Wilhelm von Kupffer,
b. 1829) are macrophages found in the sinusoids
of the liver. These cells have standard macrophage
/ monocyte specialization (i.e, receptor-mediated phagocytosis, lysosomal
digestion). Cells in this particular population of macrophages are especially
significant, with responsibility not only for cleaning bacteria out of the
portal blood stream (the "dirty" blood" from the intestine),
but also for removing worn-out red blood cells and recycling hemoglobin (a
job shared with macrophages of the spleen).
 Kupffer
cells are closely associated with the endothelial lining of the liver.
Lying along side or draped across the liver sinusoids, the Kupffer cells
are not easily distinguished from the endothelial cells.
Kupffer
cells are closely associated with the endothelial lining of the liver.
Lying along side or draped across the liver sinusoids, the Kupffer cells
are not easily distinguished from the endothelial cells.
Historical note The obsolete term reticuloendothelial system refers to the
macrophages of the liver, spleen and lymph nodes, i.e., those organs with
elaborate endothelially-lined channels supported by reticular
connective tissue. The name reflects former confusion about the
distinction between endothelial cells and the scattered population of macrophages
(monocytes, histiocytes). Macrophages can be readily labelled experimentally
through their phagocytosis of injected carbon particles. However,
endothelial cells are also labelled by the same procedure. Although
endothelial cells are not dramatically phagocytotic, they do shuttle some
materials across the endothelial lining via small endocytotic and exocytotic
vesicles.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Ito Cells
Ito cells (named after Toshio Ito) are perisinusoidal stellate cells
of the liver, located at intervals within the space
of Disse. These cells function as storage sites for fat and vitamin
A (also see PubMed).
Historical note: Although evidently included
within Kupffer's original description of Kupffer cells,
Ito cells comprise a distinct cell type (proper Kupffer cells are liver
macrophages).
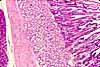
Gastric Surface Mucous Cells
 The protective epithelial cells which line the surface of the stomach
(including gastric pits) are called surface
mucous cells. These cells are critical for resisting attack by digestive
acid and enzymes.
The protective epithelial cells which line the surface of the stomach
(including gastric pits) are called surface
mucous cells. These cells are critical for resisting attack by digestive
acid and enzymes.
Any disruption of these cells' function can lead to an
ulcer. See WebPath
(low mag), WebPath
(high mag), or Milikowski & Berman's Color Atlas of Basic Histopathology,
pp. 240-241.
 The appearance of surface mucous cells is rather different from that other
mucous cells. Their nuclei are not compressed
basally (at least, not usually as much so as other mucous cells) and their
apical mucus droplets show some affinity for eosin (i.e., pink-staining in
H&E). These differences presumably reflect the fact that the mucus
secreted by these cells has a special composition to resist digestion.
The appearance of surface mucous cells is rather different from that other
mucous cells. Their nuclei are not compressed
basally (at least, not usually as much so as other mucous cells) and their
apical mucus droplets show some affinity for eosin (i.e., pink-staining in
H&E). These differences presumably reflect the fact that the mucus
secreted by these cells has a special composition to resist digestion.
 Individual surface mucous cells also differ in shape from intestinal goblet
cells. Since the mucosal surface of the stomach consists of these
cells and no others, individual surface mucous
cells cannot bulge apically like the goblet
cells.
Individual surface mucous cells also differ in shape from intestinal goblet
cells. Since the mucosal surface of the stomach consists of these
cells and no others, individual surface mucous
cells cannot bulge apically like the goblet
cells.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
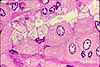
Gastric Parietal Cells
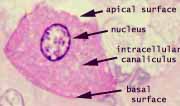
 Parietal
cells (oxyntic cells) of the stomach secrete
acid, by pumping hydrogen ions across the cell membrane. These are among
the most dramatically differentiated epithelial cells in the body, with functional
specialization reflected in their microscopic appearance.
Parietal
cells (oxyntic cells) of the stomach secrete
acid, by pumping hydrogen ions across the cell membrane. These are among
the most dramatically differentiated epithelial cells in the body, with functional
specialization reflected in their microscopic appearance.
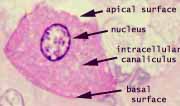 Parietal
cells are relatively large cells, with one or two oval, centrally located
euchromatic nuclei. The cytoplasm is strongly acidophilic, is
somewhat grainy in appearance, and is typically less-intensely stained in
a "halo" zone midway between the nucleus and the cell membrane.
This cytoplasmic appearance is closely associated with the parietal cell's
functional specialization for secreting acid.
Parietal
cells are relatively large cells, with one or two oval, centrally located
euchromatic nuclei. The cytoplasm is strongly acidophilic, is
somewhat grainy in appearance, and is typically less-intensely stained in
a "halo" zone midway between the nucleus and the cell membrane.
This cytoplasmic appearance is closely associated with the parietal cell's
functional specialization for secreting acid.
[Note that cytoplasmic acidophilia or basophilia in histological
preparations is no reflection of cytoplasmic pH, but only of the incidental
post-fixation staining characteristics of cytoplasmic organelles. For
example, mitochondria happen to be acidophilic. Ribosomes happen to
be basophilic.]
Pumping hydrogen ions against a tremendous concentration gradient (from pH
= 7.0 to pH < 1.0) requires energy, which in turn requires mitochondria
to produce ATP. [Consult your physiology references
for additional detail about acid production by parietal cells.]
Parietal cells contain so many mitochondria that the cytoplasm
appears to be packed with these organelles, leading to the cells' characteristic
acidophilia (mitochondria are acidophilic).
 The area of membrane surface across which ions may be pumped is substantially
increased by a deep invagination into the cytoplasm (the so-called intracellular
canaliculus). The surface area of this pocket is further increased
by microvilli.
The area of membrane surface across which ions may be pumped is substantially
increased by a deep invagination into the cytoplasm (the so-called intracellular
canaliculus). The surface area of this pocket is further increased
by microvilli.
Since the lumen of the canaliculus is extracellular, it
contains no organelles and appears less intensely stained. Thus the pale
"halo" around the nucleus gives microscopically visible evidence
of the canaliculus.
Parietal cells may be found at any level in the fundic
glands, but they are most common in the middle region.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Gastric Chief Cells
 Chief
cells of the stomach secrete the digestive enzymes
(pepsins) of the stomach and have the typical appearance of serous-secretory
epithelial cells.
Chief
cells of the stomach secrete the digestive enzymes
(pepsins) of the stomach and have the typical appearance of serous-secretory
epithelial cells.
 Secretory
vesicles (containing pepsinogen) are sometimes clearly visible in the apical cytoplasm
of chief cells. Basal cytoplasm is strongly
basophilic (especially by comparison with parietal cells), due to the presence
of the extensive rough endoplasmic reticulum that synthesizes protein for
secretion.
Secretory
vesicles (containing pepsinogen) are sometimes clearly visible in the apical cytoplasm
of chief cells. Basal cytoplasm is strongly
basophilic (especially by comparison with parietal cells), due to the presence
of the extensive rough endoplasmic reticulum that synthesizes protein for
secretion.
[Note that cytoplasmic acidophilia or basophilia in histological
preparations is no reflection of cytoplasmic pH, but only of the incidental
post-fixation staining characteristics of cytoplasmic organelles. For
example, mitochondria happen to be acidophilic. Ribosomes happen to
be basophilic.]
Chief cells may be found at any level in the fundic
glands, but they are most common in the deeper region, closer to the muscularis
mucosae.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Gastric Mucous Neck Cells
 Mucous neck cells of the stomach are inconspicuous
epithelial cells with a typical mucous-secretory
appearance. These cells are most common in the upper ("neck")
region of the fundic glands (i.e., near to the glands' openings into the bottoms
of gastric pits). Their specific function
remains unclear.
Mucous neck cells of the stomach are inconspicuous
epithelial cells with a typical mucous-secretory
appearance. These cells are most common in the upper ("neck")
region of the fundic glands (i.e., near to the glands' openings into the bottoms
of gastric pits). Their specific function
remains unclear.
 Mucous neck cells are difficult to identify in routine sections of stomach mucosa.
When the cells are neatly cut from top to bottom, they can be recognized
by the basally compressed (often wedge-shaped) nucleus and the stored mucus
that fills the apical cytoplasm. But in other random planes of section,
the poorly-stained mucus is inconspicuous and the nucleus can resemble any
of the small dense nuclei found in lamina
propria.
Mucous neck cells are difficult to identify in routine sections of stomach mucosa.
When the cells are neatly cut from top to bottom, they can be recognized
by the basally compressed (often wedge-shaped) nucleus and the stored mucus
that fills the apical cytoplasm. But in other random planes of section,
the poorly-stained mucus is inconspicuous and the nucleus can resemble any
of the small dense nuclei found in lamina
propria.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Endocrine Cells
Link to the endocrine system.
Many of the body's cells secrete substances which influence other cells,
either locally or at some distance. Cells generally regarded as endocrine
cells are those which are conspicuously specialized for this function. 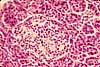 The
gastrointestinal system has two classes of such cells, the islets
of Langerhans in the pancreas and the
enteroendocrine cells in the mucosal epithelium of the stomach
and intestine.
The
gastrointestinal system has two classes of such cells, the islets
of Langerhans in the pancreas and the
enteroendocrine cells in the mucosal epithelium of the stomach
and intestine.
Pancreatic islets are covered elsewhere.
Enteroendocrine cells comprise a class of columnar epithelial cells,
scattered individually among the absorptive cells
and exocrine cells that line the mucosa of the GI tract. They are located
most commonly in the necks and deeper in gastric
glands and in the lower portions of intestinal
crypts. Each type of enteroendocrine cell is specialized
to secrete a particular hormone that influences gastrointestinal secretion
or motility. Consult your physiology text for functional details.
Enteroendocrine cells have traditionally been recognized
by their affinity for certain metal stains (e.g., see Webpath),
hence the older terms chromaffin
cells (having an affinity for chromium) and argentaffin cells
or argyrophil cells (having an affinity for silver). With sufficient
resolution, these cells can sometimes be recognized in routine light microscopic
preparations by their relatively pale cytoplasm with a broad base and a
basal concentration of secretory vesicles (in contrast to the apical concentration
of secretory vesicles for exocrine serous cells
or mucous cells). Immunocytochemical
methods are preferred for demonstrating and properly identifying the various
types of enteroendocrine cells.
Consult your histology textbook and/or atlas for additional
detail and electron micrographs of these cells.
Stem Cells
Stem cells are undifferentiated cells which remain capable of cell
division to replace cells which die. In the gastrointestinal tract,
epithelial stem cells are essential continual replenishment of the surface epithelium.
 Microscopically,
stem cells lack distinguishing characteristics. However, their activity
can be detected by the presence of mitotic
figures, the intensely basophilic masses of condensed chromation which characterize
cells undergoing mitosis.
Microscopically,
stem cells lack distinguishing characteristics. However, their activity
can be detected by the presence of mitotic
figures, the intensely basophilic masses of condensed chromation which characterize
cells undergoing mitosis.
(Other organ systems also contain stem cells, most notably
the hemopoietic cells of bone marrow. These other regions will not
be covered here.)
Stem cells of the gastric mucosa are located
at the at the top of the glands where they open into the pits. These
cells are responsible for replenishing the secretory cells of the gastric
glands and also the surface mucous cells
that protect the stomach surface. These cells are difficult to notice
and even more difficult to identify in routine histological preparations.
 Stem
cells of the intestinal mucosa line the walls
of the crypts and continually replenish
the intestinal epithelium, completely replacing all the absorptive
cells and goblet cells approximate once every four
days. These cells are inconspicuous when resting, but mitotic figures
(intensely basophilic condensed chromatin) are common and easily noticed in
the crypts of the small intestine.
Stem
cells of the intestinal mucosa line the walls
of the crypts and continually replenish
the intestinal epithelium, completely replacing all the absorptive
cells and goblet cells approximate once every four
days. These cells are inconspicuous when resting, but mitotic figures
(intensely basophilic condensed chromatin) are common and easily noticed in
the crypts of the small intestine.
The importance of stem cells in the intestinal crypts
is illustrated by recovery from cholera. The cholera toxin
kills the intestinal epithelium, leading to loss of bodily fluid across
the mucosa, copious diarrhea, massive dehydration, and death within a few
days. However, if patients can be kept hydrated for those few days,
epithelial replacement by stem cell division will restore normal function.
Stem cells of the oral cavity and the esophagus,
like those of the epidermis, are located in the basal cell layer of the stratified
squamous epithelium.
Consult your histology or cell biology textbook for additional
information about stem cells.
Tuft Cells
Tuft cells are a less familiar cell type, distinct from absorptive cells, which have a tuft of microvilli
extending into the lumen. New studies (published 2016 in Nature and in Science) have reported "an important
role for tuft cells in promoting immunity against parasitic helminths or protozoa" [PERSPECTIVE:
Science 351:1264-65].
Comments and questions: dgking@siu.edu
SIUC / School
of Medicine / Anatomy / David
King
https://histology.siu.edu/erg/gicells.htm
Last updated: 3 August 2023 / dgk
 The
apical surface area of each absorptive cell is greatly increased by
evagination into a dense array of microvilli, visible microscopically
as the brush border.
The
apical surface area of each absorptive cell is greatly increased by
evagination into a dense array of microvilli, visible microscopically
as the brush border. The
life-span of absorptive cells is short, only a few days. During
this time, the cells migrate from deep in crypts, where they are formed by
dividing stem cells, to the surface epithelium where they
eventually undergo apoptosis. Along villi, this migration is sometimes
called "the epithelial escalator." Look for apoptosis at
the tips of villi.
The
life-span of absorptive cells is short, only a few days. During
this time, the cells migrate from deep in crypts, where they are formed by
dividing stem cells, to the surface epithelium where they
eventually undergo apoptosis. Along villi, this migration is sometimes
called "the epithelial escalator." Look for apoptosis at
the tips of villi.















 In appearance, hepatocytes are boxy (cuboidal) cells with one or two large
euchromatic nuclei and with abundant, grainy cytoplasm that stains well with
both acid and basic dyes (reflecting the abundance of various cellular constituents).
Because individual liver cells have an indefinite lifespan, they may
accumulate abundant
In appearance, hepatocytes are boxy (cuboidal) cells with one or two large
euchromatic nuclei and with abundant, grainy cytoplasm that stains well with
both acid and basic dyes (reflecting the abundance of various cellular constituents).
Because individual liver cells have an indefinite lifespan, they may
accumulate abundant 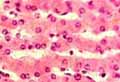




 The area of membrane surface across which ions may be pumped is substantially
increased by a deep invagination into the cytoplasm (the so-called intracellular
canaliculus). The surface area of this pocket is further increased
by microvilli.
The area of membrane surface across which ions may be pumped is substantially
increased by a deep invagination into the cytoplasm (the so-called intracellular
canaliculus). The surface area of this pocket is further increased
by microvilli.