TOP OF PAGE
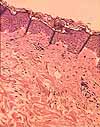
Keratinocytes
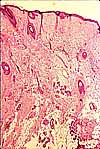
The epidermis consists primarily of keratinocytes. Scattered
among the keratinocytes are a few other cell types -- melanocytes,
Langerhans cells, and Merkel cells
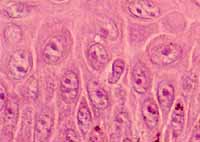
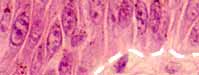
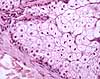
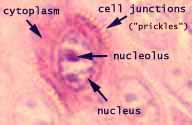 Keratinocytes,
which comprise most of the epidermis, are characterized
by numerous intercellular junctions (desmosomes), reinforced by intracytoplasmic
tonofilaments.
Keratinocytes,
which comprise most of the epidermis, are characterized
by numerous intercellular junctions (desmosomes), reinforced by intracytoplasmic
tonofilaments.
Each desmosome is one spot of attachment. At
high magnification, the desmosomes are visible as fine "prickles"
extending across the gap (intercellular space) between adjacent keratinocytes.
Between these junctions lie intercellular
channels which permit nutrients to diffuse from dermis into epidermis.
(More.)
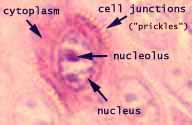
Keratinocytes in the stratum basale of the epidermis
can undergo mitosis. The formation of new cells in this basal layer
gradually pushes previously formed cells upward where they become the stratum
spinosum. As keratinocytes approach the surface of the epidermis,
they accumulate intracellular keratin and secrete a waxy material into the
intercellular space; these changes are visible in the stratum
granulosum, a distinctive layer which is diagnostic for a keratinized
epithelium. As maturing keratinocytes seal off the intercellular spaces
through which they receive nutrients, they eventually die and form the stratum
corneum, a tough and relatively inpermeable layer of hardened, dead cells.
Eventually, as cells reach the surface, they are sloughed off. The
entire epidermis above the basal layer is replenished (replaced by new cells)
within about two weeks. Replacement is accelerated by injury.
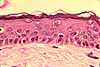
 The
stages in keratinocyte maturation appear as layers in
the epidermis, so that a section across the epidermis illustrates the
entire process.
The
stages in keratinocyte maturation appear as layers in
the epidermis, so that a section across the epidermis illustrates the
entire process.
See the Electron
Microscopic Atlas of cells, tissues and organs in the internet for (mostly unlabelled) EM images of epidermis.
TOP OF PAGE
Other epidermal cell types
 Scattered among the much more numerous keratinocytes are
several other epidermal cell types -- melanocytes, Langerhans cells,
and Merkel cells. Because these cells lack the tough reinforcement
and desmosomal attachments that characterize keratinocytes,
they commonly shrink during preparation and appear surrounded by a clear "halo".
(Together these cell types are all quite distinct from keratincytes.
But they are difficult to distinguish from one another without special techniques.)
Scattered among the much more numerous keratinocytes are
several other epidermal cell types -- melanocytes, Langerhans cells,
and Merkel cells. Because these cells lack the tough reinforcement
and desmosomal attachments that characterize keratinocytes,
they commonly shrink during preparation and appear surrounded by a clear "halo".
(Together these cell types are all quite distinct from keratincytes.
But they are difficult to distinguish from one another without special techniques.)
Melanocytes manufacture the pigment melanin.
Melanocytes appear as small cells, usually in or near the stratum
basale. They have thin cytoplasmic processes
(not evident in ordinary histological preparations) which extend between
nearby keratinocytes and serve to transfer
melanosomes (melanin-containing granules) into adjacent keratinocytes.
Because of this transfer, most pigment-containing cells in the epidermis
are normally keratinocytes rather than melanocytes.
Melanocytes may be found in places other than skin, such the choroid layer of the eye.
Melanocytes are
derived from neural crest and migrate to their final position in the epidermis.
This developmental propensity for travel may contribute to the dangerously
metastatic potential of melanomas.
Langerhans cells (named after Paul Langerhans, b. 1847)
are antigen-presenting cells which
participate in the surveillance function of the immune
system. (Antigen-presenting cells acquire foreign materials [antigens]
and pass them along to lymphocytes.) Langerhans
cells are smaller than keratinocytes, with
relatively clear cytoplasm, usually located within the stratum spinosum
or stratum basale. Langerhans cells are dendritic cells, with
extensive cytoplasmic processes extending between keratinocytes to sample
intruding antigens throughout the epidermis.
[NOTE: Please try not to confuse Langerhans
with Langhans, each of whom has an eponymous cell named after him.]
Merkel cells (named after Friedrich Merkel, b. 1845) are
small cells associated with nerve
endings in epidermis. Their function has long been uncertain,
but they seem to be involved in neural development and tactile sensation.
Recent evidence supports a role for Merkel cells in light touch, "suggesting
that these cells form an indispensible part of the somatosensory apparatus"
(Science 324:1580, 2009; also see The Journal of Neuroscience
32(10): 3296-3300, doi: 10.1523/JNEUROSCI.5307-11.2012 ). Some
uncommon skin cancers derive from Merkel cells.
See the Electron
Microscopic Atlas of cells, tissues and organs in the internet for (mostly unlabelled) EM images of Merkel cells.
TOP OF PAGE
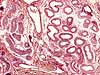
Dermis and hypodermis
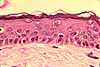
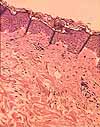 The
dermis consists of dense, fibrous connective
tissue whose predominant connective tissue component is collagen.
The
dermis consists of dense, fibrous connective
tissue whose predominant connective tissue component is collagen.
- The texture of collagen fibers
serves as the basis for recognizing two layers of dermis.
- The papillary layer of the dermis lies
adjacent to the epidermis and consists of relatively small, finely textured
collagen fibers. This layer is named after dermal papillae,
the protrusions of dermal connective tissue which indent the base of the
epidermis. Dermal papillae increase the contact area for attachment between dermis and epidermis;
they are more pronounced in thick skin.
- The reticular layer of the dermis lies
beneath the papillary layer and consists of larger, more coarsely textured
collagen fibers. ("Reticular" means "like a network"
and describes the texture of collagen fibers in this layer.)
 Like
ordinary connective tissue throughout the body, connective
tissue of the dermis serves several distinct functions.
Like
ordinary connective tissue throughout the body, connective
tissue of the dermis serves several distinct functions.
- Tough collagen fibers and
resilient elastic fibers provide mechanical
strength for skin.
Clinical note: Lines of tension in the dermis, called Langer's
lines (after Karl Langer, b. 1817), affect
healing after surgical incision. Cuts across the
lines tend to pull apart, with concommitant tendency toward tissue distortion and scarring, more so
than do cuts parallel to the lines.
- The ground substance of the
dermis serves as the substrate for diffusion of nutrients and wastes
to and from various other tissue components.
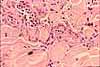
 Mast
cells, lymphocytes and macrophages
in the connective tissue carry out surveillance
for the immune system.
Mast
cells, lymphocytes and macrophages
in the connective tissue carry out surveillance
for the immune system. - Finally, the dermis together with its associated blood
vessels and nerves is capable of active response to injury, yielding the
defensive reaction of inflammation, followed
by the healing processes of growth
and repair.
Within the dermis are embedded several other structures, including epidermal
appendages (sweat glands and hair follicles)
as well as blood vessels and nerve endings.


 The
connective tissue of the dermis grades into hypodermis, without a sharp
transition or distinct boundary.
The
connective tissue of the dermis grades into hypodermis, without a sharp
transition or distinct boundary.
Over most of the body, hypodermis is characterized by adipocytes
and may comprise a thick layer of adipose tissue. In some sites
(e.g., "dimples"), hypodermis is fibrous and binds the dermis
to underlying structures. Hair follicles and sweat glands may extend into hypodermis
Blood vessels are generally larger in the deeper layers of skin, with only capillaries
in the papillary layer of the dermis.
The appearance of the skin can have considerable clinical significance.
The skin is readily accessible for examination (no invasive procedures
needed), and its color and texture can reveal much about underlying physiology.
Color: Skin is moderately transparent. Light which penetrates
the skin is reflected back from varying depths by epidermal cells, by collagen,
and by blood.
Recent research: "Shedding light on skin color,"
Science 346: 934-936
Melanin, produced by melanocytes
and stored in basal keratinocytes, contributes
a yellow/brown color to the epidermis. If the epidermis is not heavily
pigmented, light readily penetrates into the dermis.
Collagen scatters
light from the dermis without altering its color. Hence, the whiteness
of "white" skin is primarily a reflection of collagen.
Hemoglobin in red blood cells
scatters red light and is responsible for the pinkness of unpigmented
skin. The relative amount of pink in any given patch of skin reflects
how closely blood approaches the base of the epidermis (i.e., how much
collagen intervenes to scatter white light before red blood cells can
absorb the non-red colors).
Each of these elements contributes to the apparent color of skin. Variations
in skin color in different parts of the body (see regional
differences) are based on variations in these elements, most especially
the amount of pigment, the thickness of dermis, and the degree
of perfusion in dermal capillaries.
Perhaps most significantly, blood flow through the
dermis is highly variable and is regulated in response to many conditions
(heat, pain, fluid balance, inflammation, emotional reaction). Resulting
variations in pinkness can provide indicators of underlying physiology,
both locally and systemically. Obvious examples include inflammation,
overheating, dehydration, shock, and even embarrassment
(i.e., blushing) .
Texture: Skin texture is affected the thickness and smoothness
of the epidermis, by the quality of fibers in
the dermis, and by the amount of fluid in dermal connective tissue.
Because the epidermis is continually
being replenished by cell divisions among basal keratinocytes
and because this tissue is exposed to a variety of insults, the epidermis
is especially prone to disturbances of growth. See any pathology book
for examples.
The connective tissue fibers
of the skin are permanent, enduring without replacement (except by repair
after injury) throughout life. Although collagen
is quite durable, elastin commonly deteriorates
with age (and especially with repeated exposure to sunlight) and loses its elasticity. This is easily demonstrated
by a "pinch test." In youthful skin, loose skin that has been
pinched into a ridge quickly returns to its normal position when released.
Elderly skin commonly remains in its deformed position, returning
more slowly if at all.
Both edema (accumulation of excess fluid in connective
tissue) and dehydration can dramatically alter the appearance of
skin.
Skin includes several specialized structures, including epidermal
appendages (sweat glands, hair follicles,
nails) as well as blood vessels
and nerve endings which travel through the dermis.
Epidermal appendages play an especially important role in recovery from superficial
scrapes and burns. Even when the epidermis has been removed
over a fairly large area, it can grow back quickly from the epithelial cells
which remain in deeper hair follicles and/or sweat glands. Third-degree
burns are so serious precisely because tissue damage extends deep enough
into the dermis to destroy these sources of replacement cells.
TOP OF PAGE
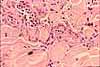
Sweat glands

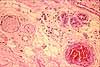
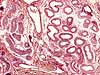
 Sweat glands are simple tubular glands lined by cuboidal epithelium. The secretory
portion of the gland lies deep in the dermis, where the tubule is twisted
into a fairly compact tangle. A duct communicates outward through the
overlying dermis and the epidermis.
Sweat glands are simple tubular glands lined by cuboidal epithelium. The secretory
portion of the gland lies deep in the dermis, where the tubule is twisted
into a fairly compact tangle. A duct communicates outward through the
overlying dermis and the epidermis.
The secretory portion of a sweat gland is comprised of cells which are larger than those of
the duct. These cells form a simple
cuboidal epithelium, along with interspersed myoepithelial
cells (which can expel sweat by contraction).
 Cells
comprising the duct, or conducting portion of the tubule, usually form a
two-layered stratified
cuboidal epithelium. These cells are usually stained more intensely
than those comprising the secretory portion of the tubule. As fluid
flows through the duct, its composition is modified by reabsorption of certain
elements from the fluid. (This is primarily a means of conserving
salt.)
Cells
comprising the duct, or conducting portion of the tubule, usually form a
two-layered stratified
cuboidal epithelium. These cells are usually stained more intensely
than those comprising the secretory portion of the tubule. As fluid
flows through the duct, its composition is modified by reabsorption of certain
elements from the fluid. (This is primarily a means of conserving
salt.)
Sweat glands are vital for thermoregulation.
They also influence water and ion balance.
The primary function for sweating is evaporative cooling
of the body. Thus, the amount of sweat is regulated as a function
of body temperature.
However, sweat also contains salt. Normally, sweat
which comes out on the surface of the skin has a lower salt concentration
than the precursor fluid produced by the secretory cells of the sweat gland.
Salt is reabsorbed by the duct of the sweat gland. The effectiveness
of this salt reabsorption is regulated by aldosterone (the hormone responsible
for maintaining electrolyte homeostasis) in response to bodily salt balance.

 There are two types of sweat glands. Ordinary eccrine sweat
glands are found over most of the body, while larger apocrine sweat
glands are found in axillary, pubic, and perianal regions.
There are two types of sweat glands. Ordinary eccrine sweat
glands are found over most of the body, while larger apocrine sweat
glands are found in axillary, pubic, and perianal regions.
Both types of sweat glands have the same
basic shape, but apocrine glands have taller cells and much larger diameter.
TOP OF PAGE
Hair follicles
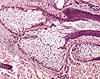
 Hair follicles are tubular invaginations lined by stratified squamous epithelium
similar to epidermis.
Hair follicles are tubular invaginations lined by stratified squamous epithelium
similar to epidermis.
Toward the bottom of each follicle, processes of cell division,
growth, and maturation similar to those in the epidermis yield a cylindrical
column of dead, keratinized cells (the hair shaft) which gradually extrudes
from the follicle. (For details, consult your histology textbook.)
 Hair
follicles are associated with sebaceous glands as
well as nerve endings and smooth muscle, which all together form the pilosebaceous apparatus.
Hair
follicles are associated with sebaceous glands as
well as nerve endings and smooth muscle, which all together form the pilosebaceous apparatus.
- A network of nerve endings
detects deflection of the hair shaft and also controls piloerection
(hair "standing on end," or "goose bumps").
- Piloerection is effected by smooth
muscle. A small bundle of smooth muscle cells called the arrector
pili ("hair erector") is attached to the connective tissue sheath around each hair follicle.
- Sebaceous glands secrete
oil into the hair follicle.
 Hair
growth is moderately complex, resulting in considerable variation in appearance
of hair follicles related to growth phase (i.e., anagen, catagen,
and telogen, or growing, regressing, and resting) as well as to body region and to
age and gender. (For additional detail, consult your histology textbook or
see here (NIH NLM).)
Hair
growth is moderately complex, resulting in considerable variation in appearance
of hair follicles related to growth phase (i.e., anagen, catagen,
and telogen, or growing, regressing, and resting) as well as to body region and to
age and gender. (For additional detail, consult your histology textbook or
see here (NIH NLM).)
TOP OF PAGE

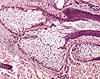
Sebaceous glands
Sebaceous glands are associated with hair follicles. The
complex of hair follicle, hair shaft, and sebaceous gland is sometimes called
the pilosebaceous apparatus.
 Histologically,
sebaceous glands are quite different from all other glands.
They are holocrine glands, which means that the whole
cell is secreted. The process of holocrine secretion is more similar
to maturation of keratinocytes than to ordinary
glandular function. Cells formed by mitosis at the base of the gland
are pushed toward the surface as new cells form below. Along the way,
the cells become packed with lipid and then die. The secretion consists
of breakdown-products of the cells themselves, which extrude into the lumen
of the associated hair follicle. So, basically, sebaceous glands are
small masses of epidermal cells in which sebum (a mixture of lipids) accumulates
rather than keratin.
Histologically,
sebaceous glands are quite different from all other glands.
They are holocrine glands, which means that the whole
cell is secreted. The process of holocrine secretion is more similar
to maturation of keratinocytes than to ordinary
glandular function. Cells formed by mitosis at the base of the gland
are pushed toward the surface as new cells form below. Along the way,
the cells become packed with lipid and then die. The secretion consists
of breakdown-products of the cells themselves, which extrude into the lumen
of the associated hair follicle. So, basically, sebaceous glands are
small masses of epidermal cells in which sebum (a mixture of lipids) accumulates
rather than keratin.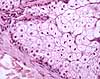
The dying cells in sebaceous glands provide a good opportunity to learn the
appearance of pyknotic nuclei, one of the more conspicuous signs
of cell death.
TOP OF PAGE
Nails
Please consult an in-depth text (e.g., Chapter 3, Histology for Pathologists,
Sternberg, 1998; newer edition: Mills, Histology for Pathologists,
3rd ed., 2007) if you desire histological details on fingernails
and toenails.
TOP OF PAGE
Innervation
The skin is richly innervated, served by a variety of sensory nerve endings
which respond to a variety of modalities (e.g., pressure, vibration, heat,
cold, itch, pain) and by motor nerve endings which control blood flow,
sweat secretion, and piloerection.
 |
 |
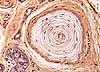
Meissner's corpuscles
|
|
 |
| Pacinian corpuscle |
For richer information on the following, see Neuroscience
Online, Somatosensory systems.
- Free nerve endings (without any conspicuous
associated structure) terminate within the epidermis,
penetrating almost to the stratum corneum.
- Merkel's
touch corpuscles (named after Friedrich Merkel, b. 1845)
are nerve endings associated with Merkel
cells at the base of the epidermis in thick
(glabrous) skin of palms and soles.
- Meissner's corpuscles (named after Georg Meissner, b. 1829)
(images at right) are encapsulated
endings in dermal papillae, most common in palmar and plantar skin, especially
in fingertips.
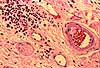
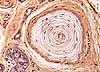
- Pacinian corpuscles (named after Filipo Pacini, b. 1812),
located deeper in dermis (image
at right), are simple nerve endings but are each encapsulated by multilamellar,
ovoid structures resembling small onions. Pacinian corpuscles respond
to deep pressure.
- Krause's endbulbs (named after Wilhelm Krause, b. 1833), or
mucocutaneous receptors, are encapsulated
endings in dermis, especially associated with lips, genital regions, nipples, and conjunctiva.
- Ruffini endings (named after Angelo Ruffini, b. 1864)
have numerous fine branches from a single axon within the fluid-filled
space of a single thin capsule.
- Hair follicle receptors
are unencapsulated nerve endings wrapped around hair follicles.
The distribution of sensory nerve endings varies from
place to place in the body (see regional differences).
Except for the characteristic capsules of Meissner's and Pacinian corpuscles,
nerve endings are inconspicuous in ordinary histological preparations of skin.
Special stains are generally used to observe nerve endings.
And except for the conspicuously encapsulated endings of Meissner's and Pacinian corpuscles,
the functional details of most sensory endings remain obscure. For
more information on tactile sensation, see Principles of Neural Science
by Kandel, Schwartz and Jessel.
Peripheral nerves (i.e., bundles of axons,
within a connective tissue sheath or epineurium) can often be found
in dermis, with smaller branches toward the surface (i.e., often near sweat
glands or hair follicles) and larger branches in deeper
layers (often running parallel to blood vessels). The following examples
show nerves in dermis.
TOP OF PAGE
Skin vasculature
The papillary layer of the dermis is richly supplied
with capillaries, while larger blood vessels may be found in
deeper levels of the dermis.
Since the skin does not have a very high metabolic demand
for nutrients and oxygen, this rich vascular network serves mainly for regulation
of body temperature. Essentially, regulation of the amount of
blood flowing through superficial capillaries allows for either conservation
or dissipation of body heat.
Arteriovenous shunts, controlled by associated
sphincters, allow blood to bypass capillaries and flow directly from arteries
into veins. These shunts occur in both deep and superficial dermis.
 The
skin is the largest organ of the body. As the primary interface between
ourselves and our environment, the skin serves several distinct functions.
The
skin is the largest organ of the body. As the primary interface between
ourselves and our environment, the skin serves several distinct functions.